
Sleep disorder: Insomnia Treatment, Symptoms, Causes & More
Living in Dubai and suffering from insomnia or sleep disorders? We show you how to have a better sleep. But be aware, its actual work!
Every third person in the UAE has at least once suffered from sleep disorders. A healthy sleep is essential for our physical and mental well being. It allows to regenerate the body and to deal with events and emotions endured during the day. But how long does a person need to sleep? Indeed there is no general valid sleep time. Each organism has a biological rhythm thus some are ‘early sleeper’ or ‘late sleeper’. The need of sleep differs according to the person, its age and sleep behavior. However, generally speaking, a person requires 7 to 8 hours of uninterrupted sleep to feel rested.
Definition
Insomnia / sleep disorders are one of the most common complaints in in the world. More than 60 million adults suffer from insomnia just in the U.S. 30% to 50% of the population is affected by insomnia or other sleep problems. Especially in Dubai – a high productive work environment – insomnia is a very common complaint.
Insomnia / sleep disorders are characterized by difficulty falling asleep and/or staying asleep, waking up often during the night, waking up too early in the morning and feeling tired upon waking. It could take a toll on the ability to function during the day and cause an irritability, depression or anxiety. For patients with sleep disorders it is often difficult to pay attention, to focus on tasks or to remember. Insomnia also could cause tension headaches and due to the reduced attention it could increase errors and accidents. Insomnia may be an independent disorder or secondary to a medical condition.
Forms
One distinguishes two forms of insomnia: The primary and the secondary Insomnia. Primary Insomnia is sleeplessness that is not directly associated with any other health condition or problem, like medical, psychiatric, or environmental causes. Secondary insomnia is a result of other causes like illness (Depression, Asthma, Arthritis, Cancer), drugs, excessive worrying, pain. Depression is a leading cause of secondary insomnia.
Moreover one distinguishes between acute and chronic Insomnia. It varies in how long it lasts and how often it occurs. It can come and go and there might be times when a patient has no sleep problems. It varies in how long it lasts and how often it occurs. It can come and go and there might be times when a patient has no sleep problems.
Types
Insomnia: A person suffers from insomnia if he/she has difficulty to falling asleep (sleep-onset insomnia); if the quality and duration of sleep is interrupted during the night or by early waking in the morning and the person is not able to get back to sleep (terminal insomnia).
Disorders of the sleep-wake-cycle: It occurs when the internal hour clock of a person to sleep at dark time and to wake up at light time is confused (e.g. due to time zone change, to shift work)
Parasomnia: It is characterized by abnormal actions or events that occur during sleep (e.g. sleep walking, sleep terrors)
Narcolepsy: It is a neurological disorder expressed by excessive daytime sleepiness.
Causes
Causes of secondary Insomnia are mentioned above. Causes of acute primary Insomnia can be emotional or physical complaint, Stress (occupational or private), Illness, Environmental factors like noise, light, or extreme temperatures that impair the quality of sleep, Medications, Interferences in a normal sleep schedule. Causes of chronic primary Insomnia can be Depression or/and Anxiety, Chronic Stress, Pain or discomfort at night.
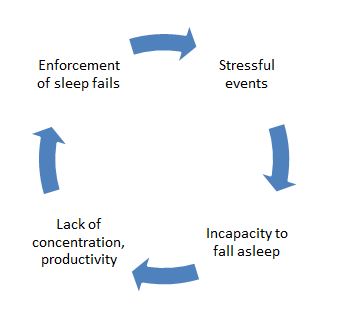
Often the feeling of tension can cause sleeplessness. Stressful events that have been occurred during the day and not been able to be broken down until the evening can prevent our sleep. A vicious circle starts as the person desires to sleep better on the next day and enforce his/her sleeps but achieves the contrary: a lack of sleep.
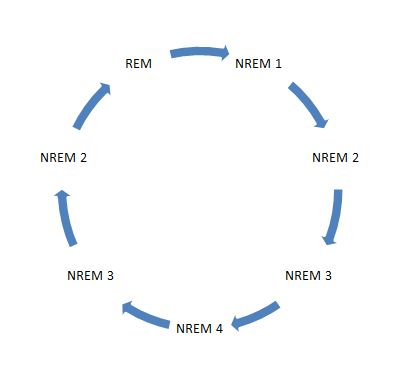 Another reason is the type of sleep. Indeed the profundity and length of a sleep characterizes its quality. Our sleep cycle distinguishes two main phases: The NREM (Non rapid eye movement) phase that has 4 stages going from light sleep to deep sleep and lasts for 90 minutes. This phase helps the body to regenerate. The REM (Rapid eye movement) phase, also known as the dream sleep, that helps to deal with events and emotions endured during the day. A person does not feel rested even if he/she slept 8 hours because the cycle was interrupted: When the person wakes up in the moment of the NREM deep sleep phase, he/she can feel not having got a good night’s rest. Also the regeneration of the body can be affected if the person is not able to reach the deep phase after going to sleep and instead wakes constantly up. The ideal cycle for a reposed sleep is shown in the diagram below:
Another reason is the type of sleep. Indeed the profundity and length of a sleep characterizes its quality. Our sleep cycle distinguishes two main phases: The NREM (Non rapid eye movement) phase that has 4 stages going from light sleep to deep sleep and lasts for 90 minutes. This phase helps the body to regenerate. The REM (Rapid eye movement) phase, also known as the dream sleep, that helps to deal with events and emotions endured during the day. A person does not feel rested even if he/she slept 8 hours because the cycle was interrupted: When the person wakes up in the moment of the NREM deep sleep phase, he/she can feel not having got a good night’s rest. Also the regeneration of the body can be affected if the person is not able to reach the deep phase after going to sleep and instead wakes constantly up. The ideal cycle for a reposed sleep is shown in the diagram below:
Finally sleep disorders can also be caused by external disruptive factors: Too low room temperature, too flat/high or too soft/hard pillow, too hard/soft mattress, a ‘low breathable’ duvet are factors of sleep discomfort. Here are some recommendations: It is recommended to air the room before going to sleep. It is important to choose a Pillow that allows the spine to be perfectly aligned. You should use a medium-firm mattress to avoid muscles pressure and offer support to back, neck and legs. If possible, choose duvets made from natural materials (feather, silk, cotton) as they are more breathable and avoid the person to perspire, wake up and have the sleep disturbed.
Diagnostics
Polysomnography is a powerful tool to diagnose sleep disorders. Polysomnography is a comprehensive recording of physiological changes that occur during sleep such as brain waves, oxygen level in the blood, heart rate and breathing rate as well as eye and leg movement. It is used to diagnose or rule out many types of sleep disorders, including Narcolepsy, Restless legs movements, REM behavior, Parasomnias, somnambulism, epilepsy related disease, snoring and sleep apnoea. On the other hand, stress related or other psychiatric disturbances may cause sleep disorders or vice versa, just as inappropriate bedding.
For all these reasons it is of the utmost importance to analyse sleep and sleeping customs thoroughly in order to determine by aid of the neurologist the individually correct diagnosis and ensuing possibilities of treatment for sleep disorders. The sole application of sleeping drugs does not represent an ideal solution but may even be dangerous because it could lead to dependencies as unwanted side-effect.
How to Prepare for the Sleep Disorder Test
There are no major preparations necessary. The patient is advised not to take any sleep medicine or drink alcohol or caffeinated beverages prior to this test.
Risk factors of the Sleep Disorder Test
Polysomnography is a non invasive procedure. There is no risk, except maybe some skin irritation caused by the adhesive used to attach the sensors to the skin. It is therefore a fabulous procedure for children too.
Mechanism of the Sleep Disorder Test
Physiologic sensor leads are placed on the patient in order to record the following:
1. EEG (Electroencephalogram)
2. EOG (Electro-Occulogram)
3. EMG (Electromyogram)
4. ECG (Electrocardiogram)
5. Airflow (thermistor or thermocouple sensor)
6. Respiratory Effort (piezo crystal effort sensor)
7. Oxygen saturation (Pulse oximeter)
Procedure of the Sleep Disorder Test
1. AT A SLEEP LABORATORY OR HOSPITAL
For the standard test, the patient – suffering from sleep disorders – comes to a sleep lab in the early evening, and over the next 1–2 hours is introduced to the setting and “wiring up” so that multiple channels of data can be recorded when he/she falls asleep. The sleep lab may be in a hospital, or in a center. A sleep technician should always be in attendance and is responsible for attaching the electrodes to the patient and monitoring the patient during the study. She must explain to the patient about the procedure to keep the patient relaxed throughout the night.
The sleep laboratory should be equipped with video cameras in the patient’s room, so that the patient can be recorded while sleeping. This allows the technician to review the tape at any time during the test and verify whether strange looking waveforms were caused by an actual arousal, a period of wake, or normal patient movements in bed.
2. AT HOME
Nowadays, neurologists may carry out home studies to enhance patient comfort and reduce expenses, which is in the best interest of any patient. The patient is given thorough instructions as to how the screening tool is used. He will then use the equipment at home in his usual sleep surroundings and return it the next day. Most screening tools consist of an airflow measuring device (thermistor) and a blood oxygen monitoring device (pulse oximeter). They are small and easy to handle and produce excellent graphs and other results. At the German Neuroscience Center our neurologists follow this new path and provide patients – suffering from sleep disorders – with a tool they can easily apply at home rather than putting the patient into an awkward situation at the clinic because they realize that especially in Arabic countries with prayer times and similar rules to follow, it might be difficult for the patient to carry out a sleep study outside their homes.
The patient will sleep with the screening device for one to three nights, and then return the device to the neurologist. The neurologist will retrieve data from the device and can make assumptions based on the information given, for example, a series of drastic blood oxygen desaturations during night periods may indicate some form of respiratory event (apnea). At a minimum, the equipment will monitor the oxygen saturation.
Sleep Disorder Test Summary
Polysomnography (PSG) has proved to be a convincing tool for enhancing our understanding of sleep and sleep disorders. It is an essential diagnostic procedure to clarify the causes of sleep disorders thus enabling the neurologist to determine an appropriate form of treatment.
Ideally, and in accordance with international guidelines, sleep studies will be carried out by neurologists in close cooperation with an ENT specialist in such cases where first results point at a serious disease, as is standard at the German Neuroscience Center GNC.
Evaluation of sleep disorders must be made more readily available to the hundreds of thousands of patients with sleep disorders who still lack diagnosis and treatment. Lack of sleep or permanently disturbed sleep will lead to reduced concentration and failing personal efficiency. This will not only gravely affect the patients’ private lives but also their daily working capacity. Sleep disorders, if not analyzed and left untreated, may lead to dangerous, even fatal, situations and social decline by, for instance, losing one’s job. Today, thanks to Polysomnography, nobody has to take such risks, since our neurologists, psychiatrists, and psychologists at the German Neuroscience Center know of many ways how to treat sleep disorders adequately after having analyzed and diagnosed the causes thoroughly.
Sleep Disorders, Treatment
There are very effective ways of treatment for sleep disorders these days. The problem is rather that patients are hesitant to search professional help. Thus a vicious circle could start where the sufferer is already afraid of going to bed. Obviously then it will be very difficult to fall asleep. If you are suffering from sleep disorders, you know what we are talking about. Specialists are using a combination of these scientifically proven treatment options for insomnia: Sleep hygiene, stimulus control, relaxation techniques, sleep restriction therapy, cognitive behavioural therapy and medications.
We would like to deliver one of these techniques to your doorstep or rather in your bedroom. Stimulus control therapy. It’s very effective and successfully used since more than 30 years. It sounds easy but it’s not. The pivotal point is your willpower to maintain these rules. It is actual work. If you don’t manage it alone, a psychologist might help you.
Rules of stimulus control therapy (Bootzin, 1980)
- Only go to bed when sleepy. Bear in mind being sleepy is not the same thing as being tired. It is important to be aware of this difference.
- Use the bed only for sleep and sexual activity. Do not engage in sleep-incompatible activity in bed such as eating snacks, watching TV or working.
- If after about 10 minutes you are unable to fall asleep or awaken, leave the bed and go to another room. Then return to bed and repeat as often as necessary until you do fall asleep. It is important to not watch the clock while doing this. It is your subjective estimate of time that is important.
- Keep a regular morning rise time no matter how much sleep you got the night before. This will help regularize the circadian (24 hour) schedule and if you don’t sleep well one night, the drive to sleep will be higher the following night.
- Avoid napping. This prevents reducing sleep drive earlier in the day that can make it harder to fall asleep at night.
Why is it working? Psychologists call it conditioning. Conditioning is a type of learning that had a major influence on the school of thought in psychology known as behaviourism. Wrong conditioning is a major problem that occurs in chronic insomnia. If you repeatedly toss and turn in your bed for hours on end, your body will eventually learn to associate your bed with stress and being awake. As a result, your bedroom will actually cause you to stay awake. The points above are trying to address this problem and to re-teach your body to associate your bed with healthy sleep. Keep in mind that it takes time and effort to make it work. Like any other form of learning. However, if this is not sufficient a combination therapy might be the right thing for you. This could include sleep hygiene, relaxation techniques, sleep restriction therapy, cognitive behavioural therapy and medication.

