Prof. Dr. med D. Claus – Neurologist Dubai

Professor of Neurology and Clinical Neurophysiology

Profile
Neurologist Professor Dubai
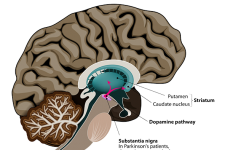
Prof. Claus, Neurologist, was head of the Department of Neurology at the Hospital of Darmstadt in Germany. In his department approximately 5000 neurological inpatients were seen each year. Part of the department was a neurological intensive care unit and a stroke unit. In addition the department included a muscle section and clinics for epileptology, and movement disorders.
Neurologist, Prof. Claus, is certified in Epileptology, Neuroradiology, Rehabilitation Medicine, Clinical Geriatrics, Electroencephalography, Electromyography, Evoked potentials, Neurovascular ultrasound, and neuromuscular ultrasound. As neurologist he regularly lectures at the University of Heidelberg.In 1990 he received the Richard Jung Award from the German Society of Clinical Neurophysiology and Neurology as a Neurologist. This was for his scientific work in the field of transcranial magnetic stimulation. Prof. Claus is an active member of the editorial board of the scientific Journal for Clinical Neurophysiology (Thieme Publisher, Stuttgart).
In 1986 he was Guest Research Fellow, Prof. J Kimura, Univ. Iowa, USA, for 6 weeks, and at the same year the General Medical Council, London, registered him as a Neurologist.
In 1987 he spent a year at the National Hospital Queen Square as a research fellow neurologist of the Royal Society, working with Professor P.K. Thomas and Professor Anita Harding amongst others. Since then he has retained his membership of the Queen Square Alumnus Association, and he is in regular contact with many physicians and colleagues from the United Kingdom. Prof. Claus was elected Corresponding Fellow of the American Academy of Neurology and of the Royal College of Physicians, London.
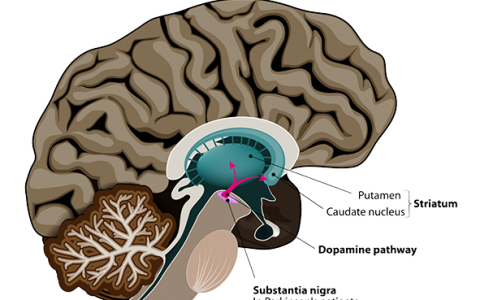
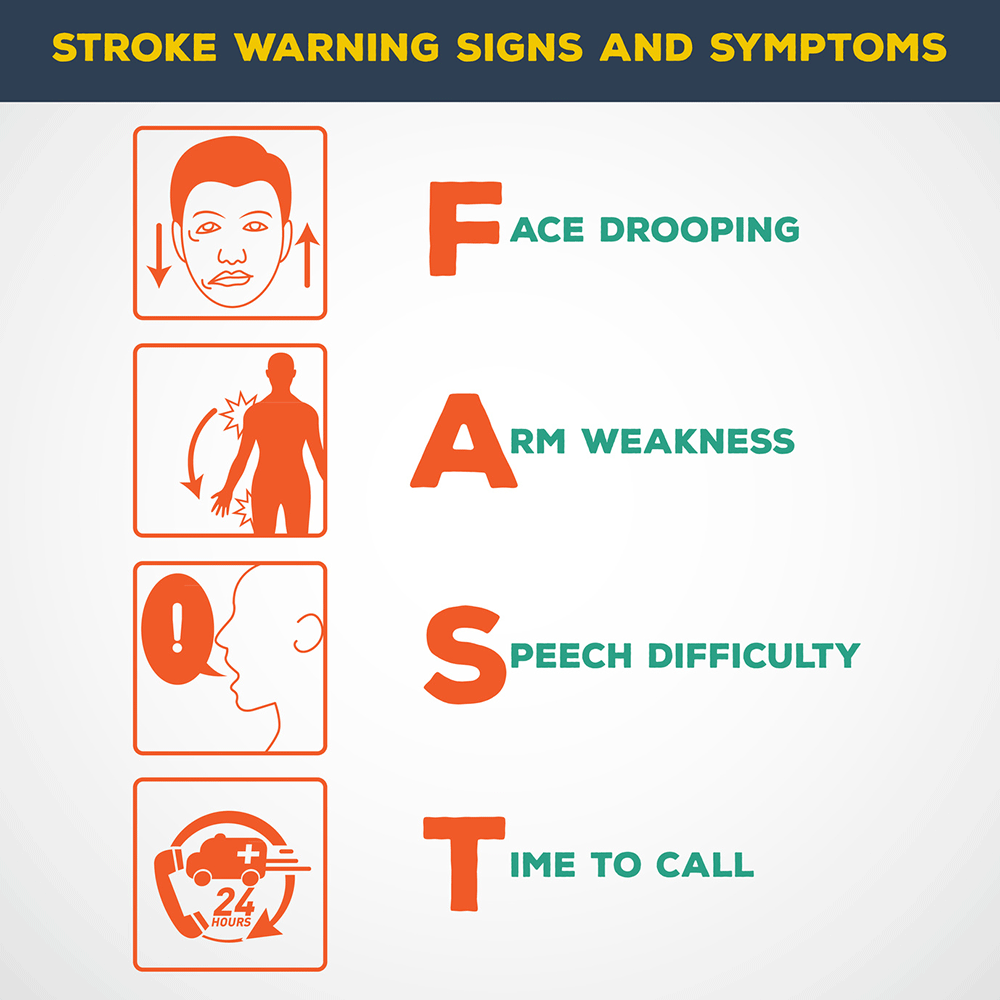
His areas of interest as a neurologist are Clinical neurology including stroke prevention, epilepsy, neurodegenerative disorders, movement disorders, polyneuropathies, and neuromuscular disorders.
Among all this Prof. Claus has a huge experience dealing with high techniques diagnostic equipments such as the colour coded duplex sonography; transcranial colour coded duplex and 24 hour blood pressure monitoring that use in Stroke prevention and Check-up and Headache work up beside the Muscle nerve investigation (neuromuscular disorders, muscle pain, entrapment neuropathies): 17-20 MHz colour coded ultrasound.
He is experienced in the use of Botulinum toxin for the treatment of dystonias, spasticity, and pain disorders.
As a neurologist, he also gives talks on various neurological topics:
Muscle pain, lumbar disc disorders, treatment of muscular strain with Botulinum toxin
Primary and secondary stroke prevention, diagnostic techniques and medical therapy
Headache – Migraine, differential diagnosis and treatment, pain treatment including Botulinum toxin in headache
Epilepsy, clinical manifestation and treatment
Peripheral nerve disorders (polyneuropathies) differential diagnosis and specific therapy
Movement disorders, clinical manifestation and treatment
Multiple sclerosis, diagnosis and therapy
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
Articles
[vc_carousel layout=”title|link_post,image|link_post,text|excerpt,link” link_target=”_blank” thumb_size=”large” speed=”2500″ autoplay=”yes” wrap=”yes”]© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
Diseases treated
Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic Lateral Sclerosis (ALS), commonly known as Lou Gehrig's disease, is a progressive neurological disorder that affects nerve cells in the brain and spinal cord. At the German Neuroscience Center Dubai, we are committed to providing comprehensive information about ALS to help patients and their families better understand this condition. In this article, we will delve into the signs, risk factors, diagnostics, treatments, and other relevant information to empower patients facing ALS.Symptoms of Amyotrophic Lateral Sclerosis (ALS)
ALS primarily targets motor neurons responsible for muscle movement, leading to a range of symptoms that gradually worsen over time. Common early symptoms include muscle weakness, twitching, and cramping, often in the arms or legs. As ALS progresses, patients may experience difficulty speaking, swallowing, and breathing. Muscle atrophy and loss of motor control are hallmarks of the disease, potentially causing mobility challenges and impacting daily life.Risk Factors of Amyotrophic Lateral Sclerosis (ALS)
While the exact cause of ALS remains unknown, certain risk factors have been identified. Although ALS can affect anyone, it is more commonly diagnosed in individuals between the ages of 40 and 70. Genetics may also play a role, with a small percentage of cases being familial. Environmental factors, such as exposure to toxins or traumatic injuries, have also been linked to a higher risk of developing ALS.Diagnostics
Diagnosing ALS requires a comprehensive evaluation, often involving various medical tests. Neurological examinations, electromyography (EMG) to assess muscle activity, and nerve conduction studies help to identify characteristic patterns of motor neuron dysfunction. Additionally, MRI and other imaging techniques can rule out other potential causes of the symptoms.Treatments of Amyotrophic Lateral Sclerosis (ALS)
While there is no cure for ALS, a multidisciplinary approach can help manage symptoms, enhance quality of life, and provide supportive care. Certain medications may slow the progression of the disease and improve life expectancy. Physical therapy, occupational therapy, and speech therapy can aid in maintaining muscle function and addressing mobility challenges. Assistive devices and adaptive technologies also play a pivotal role in enhancing independence and communication.Supportive Care and Research
ALS patients benefit from ongoing care to address the evolving needs of the disease. Support groups and counseling offer emotional and psychological support for patients and their families, helping them navigate the challenges that ALS presents. The German Neuroscience Center Dubai is actively involved in initiatives to advance our understanding of ALS, leading to improved treatment options and potential breakthroughs.Conclusion
Amyotrophic Lateral Sclerosis is a complex neurological disorder that requires comprehensive management and support. At the German Neuroscience Center Dubai, we are committed to providing patients with the latest information and personalized care to help them navigate the challenges posed by ALS. By understanding the symptoms, risk factors, diagnostics, treatments, and ongoing research efforts, patients and their families can make informed decisions and receive the support they need in their journey with ALS. Contact us today to learn more about our services and how we can assist you in managing ALS effectively.Back Pain Treatment in Dubai
Back pain is among the most common medical problem in modern society and one of the most common conditions treated by our experts. Up to 84 percent of adults experience back pain at some time in their lives. Back pain could occur at all ages with a peak around 40-50. Back pain is worldwide the most common cause of disability in persons younger than 40. Back Pain can have many different causes. Therefore, as a first step, it is important to find the underlying cause and plan the right treatment according to it. Most causes of back pain are treatable with good results and surgery can be avoided. Moreover, there are very effective measures to prevent back pain from reoccurring.Types of Back Pain
Acute vs chronic back pain: Acute back pain is most often caused by an injury or wrong movement, has a sudden onset, and lasts only hours our days. Chronic back pain is characterized as a pain lasts more than 12 weeks. Location of pain: Most common is lower or lumbar pain, but the pain can be located in the middle of the back, the upper back or neck, too. In disc related back pain and sciatica we often see a radiating pain down the legs. Severity of pain: from mild to unbearable painSymptoms / Signs
Symptoms could occur after lifting heavy items or other physical exercise. However, it can also occur without any previous activity. Peripheral nerves are having 3 functions: Pain, sensory and motor function. This explains the symptoms.- Back Pain
- Pain in the back, buttock or leg (sciatica)
- sensory loss, numbness or tingling of the skin
- Muscle weakness of the legs
- The pain could lead to muscle strain or spasm of the back muscles. Thus, the movement is impaired and the posture affected.
- A very serious symptom is called cauda equina compression. Neurologists define it as numbness of the legs, bladder / bowel dysfunction and impotence. This requires urgent surgery.
- Neck pain
- Pain in the neck, shoulder, arm, chest, Headache
- Vertigo, dizziness, giddiness, Tinnitus, Visual disturbances
- numbness in arm and hands
- weakness in arm and hands
- The pain could lead to muscle strain or spasm of the back muscles. Thus the movement is impaired and the posture affected.
Causes
Since back pain can be caused by many different underlying conditions, a thorough examination is needed to find the true cause.Some of the most common causes and underlying conditions are:
- Disc diseases
- Osteoarthritis, spondylolisthesis, fractures, osteoporosis, Spinal stenosis, Dysfunction of the joints of the lower back
- Accidents and Muscle strain
- Cancer like bony metastases and others
- Infection like osteomyelitis, tuberculosis, diskitis, epidural abscess and others
- Vascular like abdominal aortic aneurysm, epidural hematoma and others
- Rheumatologically diseases like arthritis and others
Other causes of back pain
- Pain originating in the organs close to the spine, like the stomach, kidneys, or bladder, and can radiate to your back.
- Swelling of the aorta - the main blood vessel going away from the heart - can cause back pain.
- Fibromyalgia - widespread pain and tenderness of the body - can cause back pain.
- Inflammatory diseases, stomach ulcers, and UTIs can hurt your back.
- Women: In the case of women, conditions like pregnancy and fibroids (tumours of the womb) or a disease like endometriosis can cause back pain.
- Men: In the case of men, testicular rupture or testicular torsion can be a cause.
Spondylosis
Ageing can cause our muscles, bones and the discs of the spine to weaken gradually. Everyone goes through this process of weakening of the spine, but that doesn’t necessarily become a cause of pain. The spinal discs are located between the vertebrae (bones making the spine) and act as shock absorbers. As they shrink with time, the space between the vertebrae reduces meanwhile bone spurs start developing along the edges of the vertebrae and joints. In medical terminology, this condition is referred to as spondylosis. As the discs are shrinking, the inner part of the disk, which is still more flexible, breaks thru the outer part and squeezes the nerve roots nearby. Neurologists call this a prolapsed intervertebral disk. Most common locations are the lower back, L4-L5 and L5-S1 or the neck, C5-6 and C6-7.Sciatica
Back pain is often linked to numbness, tingling feeling, or pain in the legs which is a condition called sciatica. It originates when the spinal nerve (sciatic nerve) - running down the back of the legs - gets damaged or squeezed. People with sciatica often feel more intense pain in the legs than in the back or less often feel no pain in the back. A slipped disc or an outgrowth of bone can put pressure on the sciatic nerve and cause pain or numbness along the nerve's pathway. This can cause pain anywhere from the lower back to the foot or toe.Spinal Stenosis
Another condition linked to back pain is spinal stenosis which is characterized by pain in the legs, arms, back, neck, hands, or feet. The pain can start at once and fade away or might get worse over time - depending on the location of the pain. This can be a genetic condition or might be experienced with the growing age. Our spine has a canal that contains the nerves of the spinal cord, the narrowing of this canal can result in spinal stenosis. Some people are born with a narrow canal and some may experience the narrowing of space later in life. Less space can put pressure on the nerves running through this canal, and this results in pain or numbness in different parts. Along with other areas, both or one leg can be affected, and the pain is more severe in the legs than in the back. Some people feel relieved when they sit down or walk while slightly hunching their back.Risk factors
- Obesity
- poor physical health
- poor nutrition
- Smoking
- Heavy manual labor
- Psychological reasons like depression, work related problems and others.
- Pregnancy
- Weather? No! Lower back pain is commonly associated to weather changes. But this seems to be untrue.
Diagnosis
The diagnostic procedures used depend on the patient’s complete medical history and physical examinations which determine if there is any serious underlying condition that could be causing the pain. Only after a thorough back examination and neurological tests can a healthcare provider establish the cause of back pain and the appropriate treatment. A doctor may perform several tests to identify the exact cause of back pain. These tests include;- Consultation
- Physical examination
- Neurological examination
- Electromyography (EMG): checks the electrical activity in the nerves of your spine. It is a minimally invasive technique that helps in identifying the nerve damage causing back pain.
- Nerve Conduction Velocity (NCV) Nerve conduction velocity (NCV) is a diagnostic test that measures the speed at which electrical impulses travel through nerves in the body
- X-rays: This is done to see if there is some sort of dislocation, fracture, or degeneration of bones.
- MRI: An MRI scan is usually performed to get a detailed overview of your spine. This helps in identifying even small changes and problems.
- CT scan: It is helpful in getting a complete and detailed image of your bones. It involves multiple X-rays and helps in diagnosing back pain by providing a 3-D picture of your bones.
When to See a Doctor
Back pain is common and usually gets better within a few days, but there are some conditions when you should see a doctor:- Your pain is getting worse day by day
- If it lasts for more than a week or two
- If you are unable to perform your routine tasks
- You have extreme pain that is interrupting your activities
- You are facing other health problems like fever or difficulty in penile erection
Treatment and prevention
90% of acute back pain cases will fully recover. Patients with subacute or chronic back and neck pain (3 month>) still have a favourable prognosis, however not as positive as acute back pain. Moreover, the treatment of chronic back pain or neck pain differs from treatment of acute pain. There should never be a treatment without a proper examination. Before going into detail, we will answer the most common questions patients will ask:- Do I need to get surgery? Any surgery is a potential harm to the patient. Therefore, there must be a clear indication. Luckily only less than 2% of patients suffering from neck or back pain need surgical intervention.
- Do I need to stay in bed? If the pain is acute, you will most probably lay down anyway. If your muscles cramp and the movement is impaired you don’t have much other possibilities. After the treatment started there is no beneficial effect of prolonged bed rest. Moreover, other problems like thrombosis could occur.
How to Manage Your Back Pain
There are many things you can do to ease your back pain. Staying active and maintaining a healthy lifestyle is a good way to start. Rest is important but preventing your back from any movement can worsen the pain and slow down the recovery process. Mild exercise often speeds up the recovery process. Research also suggests that your emotional responses also play a significant role in speeding up the back pain recovery process. So, one must learn to tackle the emotional challenges to get better faster. If your back pain takes too long to get better, you should see a healthcare provider.Staying Active and Exercising for Back Pain
Staying active is the first thing you can do to ease up your back pain. Regular exercise or movement makes your back flexible and keeps your spine-supporting muscles strong. This also helps in reducing pressure on your joints and bones. Your back may initially experience soreness, but it will not cause any harm. Begin with a mild exercise and gradually increase the duration and intensity. Lack of exercise or movement for a long time makes your muscles weaker and stiffer, leading to a more painful back. Regular exercise gradually eases the back pain. It also releases pain-relieving chemicals - known as endorphins - which not only help in alleviating the pain but also improve the mood. You can also take painkillers with the recommendation of your healthcare provider before performing any exercises. Gradually, you will have a stronger and more flexible back, which will reduce pain.Exercises for Back Pain
There are plenty of exercises you can choose to help relieve your back pain. Some of them are:- Swimming: It is one of the best exercises that is gentle on your back. This low-impact exercise doesn't put too much pressure on your joints, improves circulation and alleviates back pain.
- Walking: It is another way to stay active and relieve your back pain. You can choose the duration and pace according to your comfort and gradually increase them.
- Yoga: It mainly improves your muscles’ stretching and balance, which can be helpful for back pain.
- Pilates: It is also one of the recommended exercises for back pain that improves the flexibility of the body muscles and boosts core strength.
- Gym Workouts: Various workouts that are usually performed at the gym, like strength training and cardiovascular exercises can help improve overall fitness and spine health.
Medications
- Common Pain killers are reducing pain, swelling and inflammation. They are commonly used for the treatment of acute back pain. However, new studies found that these drugs are inadequate in many chronic pain scenarios, while anti-depressants and anti-convulsants can have remarkable effects on many forms of chronic bone and joint pain. Moreover, the addictive potential of opioids must be taken in consideration.
- Muscle relaxants help to release muscle spasm. Thus, the vicious circle of pain – muscle spasm – impaired movement and posture – pain – could be stopped.
- Antidepressants are commonly used and very effective for chronic lower back pain.
- Anti-convulsants (medications to prevent seizures) are successfully used in the treatment of chronic back pain.
Transcutaneous electrical nerve stimulation (TENS)
Transcutaneous electrical nerve stimulation (TENS) is a FDA approved, commonly used method in up-to-date pain management. It’s used for many forms of acute and chronic pain.Acupuncture
Acupuncture may be useful as adjunctive treatment for low back pain.Physical therapy, Massage, Occupational therapy
Physical therapy, Massage, Occupational therapy can be used to alleviate pain and restore function (but this treatment is not encouraged in the early phase of injury)Surgical therapy
Surgical therapy including Lumbar microdiskectomy,Spinal stabilization, Laminectomy, Endoscopic therapy, percutaneous arthroscopic diskectomyCBT (Cognitive Behavioural Therapy)
CBT (Cognitive Behavioural Therapy) was underestimated for a long time but as new studies prove, they are highly effective. In some cases even more effective than medication, with less side effects. A recent study published by the American Psychological Association showed when it comes to chronic pain, psychological interventions often provide more relief than prescription drugs or surgery without the risk of side effects, but are used much less frequently than traditional medical treatmentsLifestyle adjustments
Lifestyle adjustments to eliminate the risk factors, such as obesity, poor physical health, poor nutrition, smoking, heavy manual labor. Support groups are monthly meetings of 5-10 people, having one thing in common, impaired quality of life due to a chronic disease. For psychology and psychiatrist related problems, you can always consult a psychologist, psychiatrist or for counseling our psychotherapists are always available to help you. For psychology and psychiatrist related problems, you can always consult a psychologist, psychiatrist or for counseling our psychotherapists are always available to help you.Bell’s Palsy
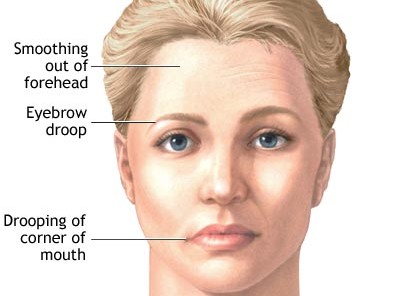
Bell's Palsy Causes, Treatment, Symptoms, Recovery & More
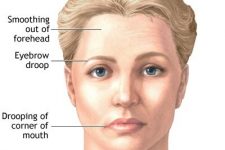
Bell’s palsy is an acute paralysis or weakness of the muscles of one side of the face. It is a relatively common peripheral nerve disorder and can affect people of all ages, but is most common between 15-45 years.
Many celebrities like Angelina Jolie, Anupam Kher, George Clooney, Pierce Brosnan suffered from Bell's Palsy.
Under the right treatment most patients have good recovery, although some are left with residual weaknessSigns & Symptoms
Bell's Palsy causes an acute paralysis of all facial muscles supplied by the seventh cranial nerve (facial nerve). It is always unilateral (one side) and involves upper and lower muscles of the face. At onset people may experiencing mild facial numbness as well. Other symptoms may include:
Read More1) Keratitis (infection of the eye) caused by the failure to close the eye
2) Loss of taste: The tip of the tongue is also innervated by the facial nerve.
3) Sensitivity to loud noises (hyperacusis): The facial nerve innervates the stapedius muscle as well.Causes
Bell's palsy is, by definition, idiopathic, meaning without a specific cause. However, it seems to be associated with certain viral infections. Herpes virus (HSV-1) could be found in 80% of patients. Other viral infections include herpes zoster virus, mumps virus, rubella virus and HIV. Lyme disease has to be taken in consideration as well.
Read MoreRisk Factors
1) Family history (10%)
2) Previous episode (8%)
3) Pregnancy (three-fold risk increase)
4) Diabetes (four-fold risk increase)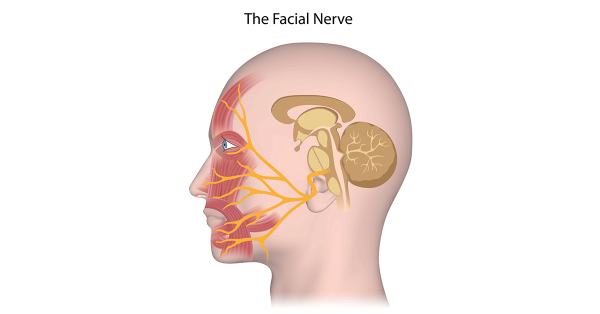
Diagnosis
For an experienced neurologist, Bell’s Palsy is mainly a clinical diagnosis. If a virus infection is suspected, blood tests may be considered. If a central paralysis cannot be excluded, a MRI might be considered. To verify the diagnosis and to predict the outcome usually a NCV (nerve conducting velocity) is performed.
Read MoreDifferential diagnosis
Important part of the diagnostic process is to exclude other serious underlying conditions leading to similar symptoms. Differentiating between central and peripheral paralysis is the first step. Stroke and multiple sclerosis as causes for central paralysis have to be exclude.
Treatment
Usually the treatment of Bell's Palsy is very effective and people have a good outcome. However, symptoms can worsen during the first days of treatment. Patients should be aware of this. The outcome of the treatment is better if the treatment is started early. Therapy may include the following:
Read More1) Injections or oral medications are improving the outcome and prognosis
2) Eye protection (a patch and eye drops preventing the eye from getting dry and developing keratitis)
3) Exercises of the affected muscles may improve the progress
4) Surgical decompression is generally not recommendedPrognosis
Usually the outcome of Bell's Palsy is good and most people recover within a few weeks. However, in 8% of the cases the paralysis is recurring.
• Good prognosis: partial paralysis
• Poor prognosis: Complete paralysis, loss of sense of taste after, pathology in the NCV test (nerve conducting velocity)
Complications
Most common complication of Bells Palsy are reinnervation problems. If the nerve is recovering and growing, it may by accident connect to other nerves resulting in malfunctions. This may include:
• Crocodile tears (crying while eating)
• Gustatory sweating (sweating while eating)
• Connection to chewing muscles (face twitching while eating)
Our Team Of Experts
Since more than ten years GNC is the leading clinic for Neurology in the UAE. All our Bell’s palsy experts are German Board Certified and have minimum professional experience of 25 years. If you are searching for the most trusted Bell’s palsy experts, you came to the right place.
We can also help you with the best psychologist, psychiatrist and psychotherapist available in Dubai, UAE.Testimonials
``The doctor is the best and everyone's very helpful``
``Excellent doctor``
``I am thankful for the service.``
``Being able to have blood tests and EEG done at the clinic itself was very helpful and convenient. This also allowed my doctor to have fast access to the test results.``
``I'm impressed by the Professor and team professionalism``
``God bless you guys wish you more of success``
``Great service``
``It was a great visit thanks! It really helped me.``
As Seen On


Carpal Tunnel Syndrome
You’ve been plagued by pain, numbness and tingling in your fingers and wrist? You are waking up at night with a “pins and needles” sensation in one hand? There might be other explanations, but the symptoms suggest you may have carpal tunnel syndrome.What is carpal tunnel syndrome?
Carpal Tunnel Syndrome (CTS) is a condition that occurs when pressure is applied on the median nerve and causes sensations of pain, numbness, tingling or weakness in the hand. The median nerve runs along the length of the arm and passes through a narrow passage in the wrist known as the carpal tunnel. If the nerve is compressed in this passage, the nerve might get damaged and symptoms occur. The median nerve is responsible for controlling the movement of your thumb and fingers, except for the little finger. Moreover, it transmits sensory information from the hand and fingers back to the brain.Common Causes of CTS (Carpal Tunnel Syndrome)
There are different causes which can lead to CTS like occupational overstressing of the hands, injuries at the wrist with malposition of the carpal bones, arthritis, pregnancy, diabetes, overweight and others. Also, a genetic predisposition is discussed. In many cases, no single cause can be identified. It may be that a combination of risk factors contributes to the development of the condition. Other causes include:- Hypothyroidism
- Obesity
- Rheumatoid arthritis
- Repetitive movements such as typing
- Diabetes
Carpal Tunnel Syndrome Symptoms
Typical symptoms are numbness or tingling in the thumb, index, middle and ring finger, later pricking and painful paraesthesias. Sometimes the whole arm up to the shoulder is affected. The symptoms are intensified by overloading the hands by repetitive manual work. At the beginning the discomfort can be reduced by “shaking” the hands. Later a persistent numbness may occur. Left untreated, carpal tunnel syndrome can lead to constant pain and to permanent nerve and muscle damage that could severely limit your ability to use your hands. When experiencing CTS in its early stages, you may notice your hands feeling numb as well as a tingling sensation. This happens during the night or after awaking in the morning; but also with certain hand positions like keyboard typing, holding a phone or reading a newspaper, cycling or motor biking. Symptoms could be worsened when holding heavy objects or bending your wrist. Many have reported that shaking their hands may relieve symptoms, but this doesn’t always make the numbness go away completely. When CTS symptoms start to worsen, you might find yourself being unable to have a strong grip when holding objects as the muscles in your hand start to shrink. You may also experience muscle cramping and pain. Other common CTS symptoms include:- Pain, tingling or numbness in your fingers and/or hand
- Weak hands
- Shock-like sensations in your fingers
- Burning or itching sensations in your palm, thumb, or index and middle fingers
- Sometimes the whole arm up to the shoulder is affected
Risk Factors
There are various factors that have been related to carpal tunnel syndrome over the years. These may not directly cause CTS, but do increase the risk of damage to the median nerve. Risk factors include:- Wrist fractures or dislocation
- Arthritis that deforms small bones in the wrist
- Gender; CTS is more common in women as the carpal tunnel area is smaller in women than in men
- Chronic illnesses such as diabetes
- Inflammatory conditions such as rheumatoid arthritis
- Medications
- Obesity
- Pregnancy
- Thyroid disorders or kidney failure
- Workplace conditions that require prolonged and repetitive movement of the wrist, such as typing
Diagnosis
When CTS symptoms develop and start to become unbearable, it is recommended that you visit a doctor. They may conduct tests such as:- Electromyograms, during which doctors will place a thin electrode into your muscle to measure its electrical activity
- Nerve conduction studies to measure the signals in the nerves of your arm and hand
- Ultrasound to look at your tissues and bones
Treatment and Prevention
Treatment for carpal tunnel syndrome will depend on the severity of your symptoms. Doctors may recommend that you:- Make changes to your daily life to avoid repetitive and strenuous wrist movements
- Exercise and stretch more often to help nerves and muscles move better on a daily basis
- Wear a splint if your doctor has advised you to prevent your wrist from moving too much
- Take anti-inflammatory drugs or steroid injections to help reduce swelling and inflammation
- If treatments don’t pan out, you may be recommended to undergo surgery to increase the size of your carpal tunnel and ease pressure on your median nerve.
- Nonsurgical Therapy: Nonsurgical therapy is possible if you have mild to moderate symptoms and the neurological examinations do not show an extensive damage at the median nerve. Medication with anti-inflammatory drugs (NSAIDs) may help relieve pain from carpal tunnel syndrome only in the short term.
- Nocturnal Splint (Wrist Splint): The most effective conservative treatment is nocturnal splinting with a specially wrist splint. If you use it, avoid wearing it all day, since that can weaken your muscles in your wrists and hands. Wearing it all night, however, is recommended. This should be done at least for 3 month.
- Surgery: If the symptoms persist or the nerve conduction velocity becomes worse, surgery has to be considered. Two main types of surgery are used to relieve the pressure on the nerves inside the carpal tunnel: Open Carpal Tunnel Release and the newer Endoscopic Carpal Tunnel Release. Both are outpatient procedures performed under local anesthesia (the surgeon cuts the ligament along the middle of the palm and inner wrist).
Lifestyle Changes and home remedies
These steps may provide temporary symptom relief:- Take short, frequent breaks from repetitive activities involving the use of the hands.
- Lose weight if you are overweight or obese.
- Rotate the wrists and stretch the palms and fingers.
- Take a pain reliever, such as aspirin, ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve).
- Wear a snug, not tight, wrist splint at night. You can find these over the counter at most drug stores or pharmacies.
- Avoid sleeping on your hands.
Alternative medicine
Integrate alternative therapies into your treatment plan to help you cope with carpal tunnel syndrome. You may have to experiment to find a treatment that works for you. Always check with your provider before trying any complementary or alternative treatment.- Yoga: Yoga postures designed for strengthening, stretching and balancing the upper body and joints may help reduce pain and improve grip strength.
- Hand Therapy: Early research suggests that certain physical and occupational hand therapy techniques may reduce symptoms of carpal tunnel syndrome.
- Ultrasound Therapy: High-intensity ultrasound can be used to raise the temperature of a targeted area of body tissue to reduce pain and promote healing. Research shows inconsistent results with this therapy, but a course of ultrasound therapy over several weeks may help reduce symptoms.
Recovery
Most people make a full recovery, but in some cases (fewer than 5 percent) carpal tunnel syndrome recurs after surgery. This happens more commonly following the endoscopic procedure, which often doesn’t open up the tunnel as fully as open release.Summary
If you are experiencing symptoms of carpal tunnel syndrome and you are searching for the most experienced neurologist to diagnose the condition and provide the best treatment, the German neuroscience Center is your clinic of choice. Since more than 15 years GNC is the leading clinic for Neurology in the UAE. All our Carpal Tunnel experts are German Board Certified and have minimum professional experience of 25 years. If you are searching for the most trusted Carpal Tunnel experts, you came to the right place. Book your appointment hereDementia & Alzheimer’s Disease
Disease
Alzheimer Dementia in Dubai
You fear having Alzheimer’s Dementia? You are suffering from memory loss? You have difficulties to concentrate? Don´t be afraid. To forget things doesn’t mean you are already suffering from Alzheimer Dementia. But what is Alzheimer Dementia actually?
Definition
Alzheimer´s Dementia is a chronic disease of the brain which starts slowly with mild symptoms. One symptom alone is not enough to justify the diagnosis. To forget some things some time does not make an Alzheimer´s Dementia. With ongoing age it is totally normal that your memory becomes worse. When you are 60 years it is more difficult to memorize information than with 50, and with 70 it is more difficult than with 60. That means you forget always a bit more becoming older in a natural way. It is very individual how much and how fast this process is ongoing. This depends on your gens, your general health situation, your environment you live in and your education. In scientific papers is was found that people with high education, university degrees or a sophisticated job, so called “brain workers”, get Alzheimer´s disease more seldom and later than people who work more physically. Our brain has a lot of resources to compensate deficiencies. And a well-trained brain does it better than a “lazy” brain.
Causes
There is not only one disease causing dementia. There are different kinds of dementia diseases like Alzheimer, vascular dementia or Lewy Body Disease Dementia. The syndromes of dementia can also be caused by other diseases like stroke, Parkinson, Hydrocephalus, brain tumor and others. It is the task of a neurologist to find out whether a person is suffering from dementia and if so, which kind. The most common dementia disease is the Alzheimer´s disease. Second most common form of dementia is the vascular dementia or a combination of Alzheimer’s Dementia and Vascular Dementia.
Symptoms
In early stages of Alzheimer´s Dementia patients are not only suffering from decline of memory but also other symptoms. People seem to be depressed because they realize their increasing problems. They feel tired, exhausted and try to avoid intellectual demanding tasks. Already in early stages of Dementia people are changing their behaviour. They are losing interest in things which were important for them before, like their job or hobbies. Patients suffering from dementia are avoiding social contacts, they want to be alone or only with very close persons like family members. The surrounding feels that something is wrong. First it is yet too little to talk or to worry about. There are always excuses to explain the changes. Then when the difficulties become more evident people feel unsecure how to talk about. Alzheimers Disease is stigmatized and for both sides it is difficult to face the facts. For the suffering person the same as for the family members or friends.
Diagnosis
It is important to have a clear diagnosis to either stop worrying or to take action. However, in early stages it can be difficult to differentiate between forgetfulness of age and an early stage of a dementia disease. There are special cognitive tests a neurologist can apply to find out whether the memory alteration is still in age range or not. If there are symptoms of an alteration more than “what is allowed”, further investigations have to be done.
Other diseases like depression, burn out syndrome caused by too much stress, physically exhaustion and other corporal diseases have to be excluded. But how to find out whether a person is suffering from dementia?
First of all go to your neurologist and talk to him about your problems. Already by talking to a patient the doctor gets a first impression. He doesn´t only hear the complaints themselves. Important are also the duration and the progression of the problems. The way how a person speaks, the signs of memory disturbances in conversation, indication of aphasia, disturbance of time or local orientation, all this might already show first straits of a beginning dementia. The doctor also watches the spontaneous behaviour to form his opinion weather it is adapted to the situation or not. It is also important to listen to family members or other close persons. Maybe they have more information the patient eventually already forgot. Or they have another view of the changes the patient did undergo.
Next step are different cognitive tests. For example the worldwide used MMSE (Mini Mental State Examination), a psychometric test to prove orientation, retentiveness, alertness, speech, memory and other function. The neurological examination gives information about the different systems of the brain, peripheral nerves and muscles. Reflexes, speech, gait and locomotor system sensibility, vision, balance and the cranial nerves are checked. It is important to look whether there are any signs which could give an advice for another disease than dementia causing the problems. Blood tests, more seldom examination of the CSF (cerebrospinal fluid) were done. The CSF is the liquid the brain and the spine are covered with all over. In this CSF special peptides can be found which indicate an Alzheimer Disease (Tau-peptide, A beta-peptide).
EEG (electroencephalography) is an examination which does not hurt, comparable to the ECG (electrocardiogram) of the heart. It gives a good overview of the global cerebral function. Other electrophysiological test like AEP (acoustic evoked potentials) or SEP (sensible evoked potentials) can give more information about a lesion in the nervous system to exclude another disease. Also ultrasonic investigations of the cerebral blood flow are part of the diagnostic procedures. The neurologist will send the patient to the imaging of the brain by MRI or CT. In early stages of dementia there are no specific signs for the disease. In more progressed stages you can find signs of atrophy in special parts of the brain (in the temporal area hippocampussklerosis). But the most important reason for the imaging in early stages is again to exclude other diseases which have to be treated in a different way and which might be healed.
Therapy
Therapy of Alzheimer disease is possible. With medication it is achievable to decelerate the progress of the disease, to stabilize the memory, concentration and basic life skills. In Alzheimer Disease nerve cells and nerve cell connections decay which cannot get restored. In consequence of the decay of the nerve cells the messenger substance Acetylcholine decreases. A special kind of medication, the so called “cholinesterase inhibitors”, compensates partly the deficit. By this the information processing improves again. There are other substances which influence the cerebral metabolism in a different way which might also have stabilizing effects on the cognitive functions. Coexisting symptoms like depression, sleeping disorders, anxiety or restlessness have to be treated with other drugs beside the special dementia medication.
Caregivers
Very important is the right contact and handling with the affected person. Lots of patience and sympathy, a quiet surrounding and good information for understanding the disease and the behaviour of the patient are absolutely essential. It is difficult and very exhausting to care for somebody in a more advanced stage when the person needs help in daily activities, in personal hygiene, in nutrition and needs observation the whole day. The family should use all the help and frontline services they could get or attend support groups.
Other than that if you think your problem can be solved by a psychiatrist or a psychologist, you can book an appointment with them as well.© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
.
Double Vision – Diplopia
What is Double Vision?
Patient with double vision see two images of a single object either permanently or intermittent. Double vision is also known as Diplopia. The displacement may be horizontally, vertically or diagonally. The perception of two images can also be overlapping. The symptom of double vision is to take seriously, since some causes need urgent medical treatment.
Symptoms
The symptoms of double vision can vary as described above but depending on the cause, other symptoms may be present with double vision, such as:
• Misalignment of one or both eyes
• Pain with the eye movements in one or both eyes
• Pain around the eyes, such as in the temples or eyebrows
• Headache
• Nausea
• Weakness in the eyes or anywhere else
• Droopy eyelidsCauses
There are many possible reasons for double vision. If the double vision is long-lasting or keeps coming back, reasons for it can include:
• Nerve problems: Multiple Sclerosis, Guillain-Barre syndrome, Diabetes
• Cornea problems: Herpes zoster, Dryness of the cornea
• Lens problems: Cataracts
• Brain problems: Stroke, Aneurysm, Migraine, Brain tumor, Head injury
• Muscle problems: Myasthenia gravisSince the reasons for double vision could be life-threatening, it is very important to consult a Specialist if the symptoms do not stop.
Types
There are three types of double vision: Binocular double vision, monocular double vision and physiological double vision. The eyes of patients with binocular double vision do not work together properly and the double vision will disappear if the patient covers one eye. Monocular double vision occurs when the double vision continues when the unaffected eye is covered. In physiological double vision background objects the patient does not focus on appear doubled. This vision problem often goes unnoticed because the patient's brain can usually compensate for this type of double vision.
Treatment
As many different diseases could lead to the symptom of double vision it can be difficult to find out what the actual cause is. It is important to have a comprehensive examination to determine the cause of double vision. In fact, the condition may be a matter of life or death, such as a brain tumor or aneurysm. Some conditions causing double vision are difficult and sometimes impossible to fix. Some strokes and nerve palsies cause fluctuating double vision that can't be measured accurately enough to correct.
To diagnose double vision and to find out the reason for this symptom the Neurologist will use multiple methods such as blood tests, a comprehensive neurological exam, and possibly imaging studies like CT and MRI. The treatment depends on the findings. If weak eye muscles are the cause for double vision a surgery may help. If Myasthenia gravis or Diabetes is the reason medications will help.
Epilepsy, Seizures, Convulsions
Epilepsy, Convulsions, Seizures, Fits
Epilepsy, Convulsions, seizures or fits are some of the most common neurological disorders, with an annual incidence of 35 to 52 cases per 100,000 persons. It is a central nervous system disorder that affects the nerve cell activity in the brain characterized by the presence of recurrent, unprovoked seizures.
The patient has a propensity to manifest recurrent episodes of disturbed behavior symptoms and sensations, including loss of consciousness. Seizures or convulsions can have profound physical and psycho-social consequences. However, one single seizure or fit does not indicate Epilepsy.
The disease can only be diagnosed if there is an underlying tendency toward recurrent, unprovoked seizures or fits.
Causes
Epilepsy has no identifiable cause in about half of those with the condition. Specialists speak about symptomatic Epilepsy if they identify a cause like a brain tumor. The most common causes of Epilepsy include:
Read MoreCauses
• Genetic influence
• Congenital abnormalities
• Antenatal or perinatal injury
• Infections such as meningitis, AIDS and viral encephalitis
• Cerebral tumors
• Traumatic brain injury
• Vascular causes (eg, stroke, vascular malformations, cerebral venous thrombosis)
• Inflammatory conditions (eg, vasculitis)
• Alzheimer disease, multiple sclerosis, and other neurodegenerative disorders
Signs & Symptoms
Specialists differentiate between focal or generalized seizures, based on how the abnormal brain activity begins. A focal seizure is characterized by an abnormal activity in just one area of the brain and it could include the loss of consciousness. Generalized seizures are...
Read MoreGeneralized seizures are the most common seizures and involve all areas of the brain and could include symptoms like staring into space or subtle body movements, stiffening of the muscles, a loss of muscle control and an abrupt loss of consciousness, body stiffening and shaking, and sometimes loss of bladder control or biting the tongue.
The general signs and symptoms of a seizure may include:
• Temporary confusion
• A staring spell
• Uncontrollable jerking movements of the arms and legs
• Loss of consciousness or awareness
• Psychic symptoms
Patients may experience an “aura” just before the seizure starts. They may feel “strange”, dizzy or nauseous and can experience changes in mood, visual perception, auditory perception or unspecific symptoms.
Classification
Epilepsy or Seizures are classified as (ILAE):
Read MoreGeneralized seizures
• Tonic–clonic (in any combination) seizures
• Clonic seizures
• Tonic seizures
• Atonic seizures
• Myoclonic seizures
• Myoclonic seizures
• Myoclonic atonic seizures
• Myoclonic tonic seizures
Absence seizures
• Typical
• Atypical
• Absence with special features
• Myoclonic absence
• Eyelid myoclonia
Focal seizures
Unknown seizures
• Epileptic spasms
Diagnosis
Diagnosing Epilepsy is a three-step process involving clinical identification of a possible seizure, consideration of differential diagnoses, and classification of the seizure. The Neurologist will...
Read MoreThe Neurologist will test behavior, motor abilities, mental function and other areas to diagnose the condition and determine the type of epilepsy the patient may have. Moreover, the examination include a blood test, an EEG (Electroencephalogram) and a neuropsychological tests, in which the Neurologist assess thinking, memory and speech skills of the patient to determine which areas of the brain are affected.
Treatment
Most people with Epilepsy can become seizure- or fit-free by taking one anti-seizure medication, called anti-epileptic medication.
The treatment of Epilepsy involves...
Read MoreThe treatment of Epilepsy involves first the establishment of the correct diagnosis and the identification of the syndrome/seizure type. In the second step the Neurologist will determine if medication is necessary and the last step will be to select the right medication. The selection of the right medication is very complex and needs to be individualized on the basis of the type of Epilepsy, patient characteristics and coexisting medical and psychiatric conditions.
However, due to the drug development of recent years there are very efficient possibilities to treat patients with Epilepsy so effectively that the majority can lead an entirely normal life without any seizures or convulsions at all. In severe cases neurosurgical interference may offer help.
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
Our Team Of Experts
Since more than ten years GNC is the leading clinic for Neurology in the UAE. All our Epilepsy experts are German Board Certified and have minimum professional experience of 25 years. If you are searching for the most trusted Epilepsy experts, you came to the right place.
We can also help you with the best psychologist, psychiatrist and psychotherapist available in Dubai, UAE.Testimonials
``The doctor is the best and everyone's very helpful``
``Excellent doctor``
``I am thankful for the service.``
``Being able to have blood tests and EEG done at the clinic itself was very helpful and convenient. This also allowed my doctor to have fast access to the test results.``
``I'm impressed by the Professor and team professionalism``
``God bless you guys wish you more of success``
``Great service``
``It was a great visit thanks! It really helped me.``
As Seen On


Book Appointment
Memory Loss, Memory Problems & Forgetfulness
Memory loss and memory problems such as Forgetfulness can be concerning, affecting various aspects of daily life. Prompt medical evaluation is crucial when encountering memory problems. As a premier neurological center in Dubai, the German Neuroscience Center is committed to providing comprehensive information about memory issues. In this article, we delve into the signs and symptoms, risk factors, causes, diagnostics, treatments, and other relevant information for patients experiencing memory challenges.Memory Loss: Signs and Symptoms
Memory issues can manifest in several ways, with varying degrees of severity. Common signs and symptoms include:- Forgetfulness: Frequent forgetfulness of recent events, appointments, or conversations.
- Difficulty Concentrating: Struggling to focus on tasks, making decisions, or following conversations.
- Confusion: Feeling disoriented or confused about time, place, or people.
- Misplacing Items: Frequently losing or misplacing items in unusual locations.
- Repetitive Questions: Asking the same questions repeatedly within a short span of time.
Risk Factors for Memory Problems
Certain factors increase the likelihood of experiencing memory problems, including:- Age: Advanced age is a common risk factor for cognitive decline and memory issues.
- Medical Conditions: Conditions like Alzheimer's disease, vascular dementia, and mild cognitive impairment can contribute to memory problems.
- Family History: A family history of cognitive decline or neurodegenerative disorders can increase the risk.
Common Causes of Memory Issues
Memory problems can stem from various underlying causes:- Neurological Conditions: Neurodegenerative disorders like Alzheimer's and Parkinson's disease can affect memory.
- Depression and Anxiety: Mood disorders can impact memory and cognitive function.
- Medications: Certain medications have cognitive side effects that affect memory.
- Sleep Disorders: Inadequate sleep or sleep disorders can impair cognitive function.
Diagnostics and Evaluation
Diagnosing memory problems requires a comprehensive evaluation, including:- Medical History: Gathering information about medical conditions, medications, and family history.
- Cognitive Tests: Assessing memory, attention, and problem-solving skills through specialized tests. At the German Neuroscience Center we offer the most advance neuropsychological testing to detect early memory loss and mild cognitive impairment.
- Imaging: Brain imaging techniques like MRI and PET scans can reveal structural abnormalities.
- EEG (Electroencephalography): EEG measures the electrical activity of the brain by recording the signals produced by neurons using electrodes placed on the scalp. This activity is displayed as wave patterns, which provide insights into brain function and potential abnormalities. EEG is a non-invasive procedure that is safe and painless, making it a valuable tool for diagnosing and monitoring dementia. Different types of dementia, such as Alzheimer's disease, vascular dementia, and Lewy body dementia, often exhibit specific EEG patterns. EEG can aid in distinguishing between these different forms of dementia based on the unique electrical signatures associated with each type.
- Laboratory Tests: Blood tests can identify underlying medical conditions contributing to memory issues.
Treatment Approaches for Forgetfulness & Memory Loss
The approach to treating memory problems depends on the underlying cause and severity:- Lifestyle Modifications: Adopting a brain-healthy lifestyle with regular exercise, a balanced diet, and adequate sleep.
- Cognitive Rehabilitation: Engaging in cognitive exercises to improve memory and cognitive function.
- Medications: In some cases, medications can help manage symptoms or slow the progression of underlying conditions. Lately some promising drugs received the FDA approval and can be used depending on the individual case.
- Therapies: Behavioral therapies, counseling, and support groups can aid in coping with memory challenges.
When to See a Doctor
Prompt medical evaluation is crucial when encountering memory problems:- Persistent Symptoms: If memory problems persist or worsen over time, consult a doctor.
- Disruption in Daily Life: If memory challenges hinder daily tasks, work, or relationships, seek medical attention.
- Sudden Changes: Rapid onset of memory issues or cognitive decline requires immediate medical assessment.
- Concerns about Loved Ones: If you notice memory problems in a family member or friend, encourage them to seek help.
Conclusion
Memory loss and memory problems can impact individuals of all ages, affecting daily functioning and quality of life. At the German Neuroscience Center Dubai, we offer specialized care and support for those experiencing memory challenges. By recognizing the signs, understanding risk factors, and seeking timely evaluation and treatment, individuals can proactively address memory issues and enhance their cognitive well-being. Our dedicated team of neurologists is committed to providing personalized care to help patients navigate the journey toward improved memory health. Contact us to book your appointment now.Migraine / Headaches
Disease
Migraine Headache
Are you suffering from headaches? You are not alone! Headache is a widespread disease and one of the most common reasons to visit a Neurologist in Dubai. It occurs in different types and strengths and can impair the quality of living substantially. It is possible to do something against it. But before a therapy can be started it has to be found out what the reason is and a correct diagnosis has to be made.
Types of headaches
There are many types of headaches. The most common are the primary headaches like migraine, tension headache or cluster headache or an analgetic headache. Your neurologist has to know how your headache feels like, where it starts; whether there are accompanying symptoms, how long it lasts and how often it occurs. Then he will do different medical examinations. After he knows the diagnosis he can give you an advice for the right treatment. Treatment is possible!
Migraine
Migraine is one of the most frequent neurological diseases. Around the world about 10 percent of the adults are suffering of migraine, more women than men. The difference between the genders has most likely hormonal and genetic reasons, neurologists assume. Typically it starts in adolescence. After the 50th year the frequency declines again.
The duration of a pain attack is between 4 to 72 hours. The frequency varies between once a year up to twice a week. The pain is moderate up to very violent. The characteristic is mostly pulsating and only on one side of the skull; but in some patients also on both sides. One side is more affected than the other. Very often people are having accompanying symptoms like nausea, vomiting, visual problems and are very sensitive against light, noise and odour. By physical exercises the pain increases.
A typical migraine attack proceeds in 4 phases. During the lead time there exist no pains yet. There could be depressive reactions, irritability and agitation. It’s important to report also sensations like these to your neurologist; even if you think it has nothing to do with the pain itself. Concentration might get reduced; people feel tired and have to yawn a lot. Oedema, constipation or a craving for sweet or greasy food may occur. The second phase might be an aura. Quite often there are visual problems with scintillating scotomas or double vision. But it also can be sensibility disturbances or movement and speech problems. An aura keeps from a few minutes up to one hour.
The third phase neurologists call the headache phase. The pulsating pain starts very often in the neck, spreads over the back of the head and settles behind the eye or at the temple. Most attacks are accompanied by vegetative symptoms. The whole body is affected. Some people are not able to continue their work. They have to lie down. They seek quietness and darkness, don`t want to hear or see anything or anybody. The duration of the headache might be up to 3 days if the attack is not interrupted by medication. Hours or 1-2 days after a migraine attack (4th phase) people feel tired and exhausted, concentration is still reduced, mood might be swinging.
Causes
It is a temporary dysfunction of the brain. During a migraine attack the blood vessels of the cerebral membrane are widened and inflamed. The nerve fibres around the vessels are irritated so heavily that they send pain signals.
There are different migraine triggers like stress, menstruation, alcohol, especially red wine, disturbances in the sleep-awake-cycle, irregular meals, weather changes, light stimulus, odour or pain in the neck. These triggers are very individual and vary even in one individual from time to time. But these triggers are not the causes of the disease they just stimulate it.
Treatment
Nowadays neurologists are using very effective and fast treatment options for migraine headaches.
If you think that visiting a neurologist might not fix what you're going through. GNC Dubai is providing one of the best psychiatrists in Dubai, psychologists in Dubai and psychotherapists in Dubai who can help you find the core reason and in fixing it.
Migraine treatment without medication:
1. Reduce stress factors as much as possible
- Learn good time management: plan your day schedule. Don`t forget enough time for brakes.
- Learn to say “No”.
- Don`t spread yourself too thin. Not everything has to be done right away.
- Think: “nobody is perfect!”
- Take life easier, enjoy it.
2. Relaxation
Proceedings for recreation as Yoga, autogenic training or progressive muscle relaxation techniques help, but have to be done regularly
3. Psychotherapy
Research could show that Cognitive Behavioral Therapy (CBT) has a positive impact on migraine patients. Even consulting a patient is able to reduce the frequency of migraine attacks. Therefore CBT was included in the Guidelines of the German Headache and Migraine Association.
4. Endurance sports
Endurance sports like cycling, walking, jogging or swimming are good. But it is important to exercise regularly, at least three times a week for about 30 minutes.
5. Sleep
Constant sleep-awake cycle, also during the weekend. And eat and drink with regularity.
6. Triggers
Avoid your personnel migraine triggers.
Migraine treatment with medication
1. Therapy of the acute migraine attacks
There are different types of medication to treat the acute attack. In easier cases common painkillers can be enough. A combination with a medication against nausea can be given. But mostly stronger medication is required. Special migraine drugs can ameliorate the attack within 2 hours in most patients. This kind of medication needs to be prescribed by a neurologist. The medication has to be taken as soon as possible. Then it helps the best. But be careful. You should not take any painkiller more often than 10-12 times a month. Otherwise there is the danger to develop an analgesic headache, which means headache by the medication itself!
2. Migraine Medical prophylaxis
In severe cases it is useful to take special medication every day to reduce the number of attacks, the length of the single attack or to improve the effect of the acute medication. This medication has to be taken for at least three quarters of a year, sometimes longer. Your neurologist will find out which medication will be the best for you and will supervise you through the therapy.
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
Multiple Sclerosis
Disease
What is Multiple Sclerosis?
Multiple Sclerosis (MS) is an autoimmune disorder in which the immune system of your own body attacks the nerves and especially their myelin sheaths. Myelin damage disrupts communication between nerve cells. Thus functions controlled by nerves could be disabled. As the nervous system is controlling almost all functions of the human body, Multiple Sclerosis may manifest itself through various symptoms. That’s why diagnosing MS is difficult and sometimes takes years. It is an unpredictable, often disabling disease and primarily occurs in young adults between the ages of 20 and 40. MS is twice as common in women as it is in men.
The cause of Multiple Sclerosis is not known but exogenous and endogenous predisposing factors may play a role. Although there is no cure for Multiple Sclerosis treatments can help speed recovery from attacks, modify the course of the disease and manage symptoms.
Multiple Sclerosis and Vitamin D
Vitamin D plays a part in regulating the immune system in the human body. As Multiple Sclerosis is an immune disease, Vit D could have a protective/modulating effect that influences the disease positively. read more
Multiple Sclerosis in UAE | Too Less Sun???
New Australian study showed again the link between too less sunlight / Vit D Deficiency and Multiple Sclerosis. But do we have too less sunlight in the UAE? Since 1974 (Goldberg) researchers are studying the link between too less sunlight and Multiple Sclerosis.
Multiple Sclerosis and Smoking
Studies could show that smoking and passive smoking are risk factor to develop MS. Moreover, patients with MS have a worse prognosis if they smoke compared to non-smoking patients. Furthermore MS drugs are not as effective if patients are smoking. Bottom line: Stop Smoking!
Symptoms
Multiple Sclerosis is often characterized by a relapsing-remitting course, with new symptoms that develop over days or weeks and usually improve partially or completely, followed by a quiet period that can last months or even years.
The signs and symptoms of Multiple Sclerosis vary with one or several of the following:
- Visual blurring, Vision loss, Double vision, pain behind the eye (optic neuritis) The risk to develop MS in the next 15 years is 50%!
- Sensory disturbances, numbness, tingling, pain
- Weakness in limbs, gait problems, incoordination, dysarthria and intention tremor
- Bladder or bowel dysfunction
- Slurred speech
- Dizziness
- Fatigue
Diagnosis
Diagnosing early MS stages can be difficult. MS symptoms can be presented by a variety of other diseases as well. A comprehensive neurological examination should be done in order to rule out other conditions that might produce similar signs and symptoms. The examination includes blood tests, a MRI of the brain and spine and a spinal tap (lumbar puncture) in which a small sample of fluid is removed from the spinal canal for laboratory analysis. This sample can show abnormalities in white blood cells or antibodies that are associated with MS. Moreover, the Neurologist will check motor strength and sensation in all limbs.
Treatment
The treatment of MS is very important even though Multiple Sclerosis is a chronic, potentially debilitating disease with no cure. The treatment focusses on reducing the frequency of relapses and speeding recovery from them. The aim is a slower disease progression and the management of the symptoms. It should be coordinated in consultation with a Neurologist specialized in MS.
There are special medications for the treatment of acute attacks which reduce nerve inflammation. Other medications can lower the relapse rate and reduce the rate of formation of new lesions. Just recently new drugs have been approved for the treatment of MS.
Besides the necessity to apply the appropriate medication in order to alleviate symptoms like palsies, pains, vision disorders, blindness and other neurological symptoms, there are also physiotherapy and other therapeutic measures that can be helpful. However, some patients have such mild symptoms that no treatment is necessary.
Living with Multiple Sclerosis
In order to relief the signs and symptoms of Multiple Sclerosis the patient should try to get plenty of rest and relaxation. Meditation and or deep breathing may help. Moreover, regular exercises can help improve strength, muscle tone, balance and coordination. Swimming, walking, stretching, low-impact aerobics, stationary bicycling, yoga and tai chi are mild to moderate exercise recommended for MS. Exercises also relieve stress which may trigger or worsen signs and symptoms. A balanced diet low in saturated fat but high in omega-3 fatty acids, such as those found in olive and fish oils, may also be beneficial. Studies also suggest that vitamin D may have potential benefits for MS.
If you think that you want to fix something else related to your mental health. GNC Dubai is providing one of the best psychiatrists in Dubai, psychologists in Dubai and psychotherapists in Dubai who can help you find the core reason and in fixing it.MS Support Group Dubai
I've multiple sclerosis but do I look scared?
Young woman with debilitating disease launches forum to help fellow patients. Supported by the German Neuroscience Center the twenty-eight-year-old multiple sclerosis patient Maha Abbas is launching an MS Talks Forum at Dubai's Urban Bistro restaurant this month end to raise awareness about the disease XPRESS, October 14, 2015, Sharmila Dhal, Chief Reporter Dubai: Maha Abbas, 28, is a multiple sclerosis ( MS) patient with a difference.
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
Myasthenia Gravis
Myasthenia Gravis
Myasthenia gravis is an autoimmune disease that causes muscle weakness. The body is producing antibodies which are attacking the junction between nerve and muscle.
Signs & Symptoms
Most common symptoms of Myasthenia gravis are ocular symptoms (50%) of Drooping of the eyelids (ptosis), double vision (diplopia) and blurred vision. The disease can generalize including symptoms like weakness of facial and extremity muscles. Moreover, patients could have difficulties in chewing, swallowing and speech. Respiratory weakness may produce acute respiratory failure.
Read MoreThe symptoms of Myasthenia gravis are negatively influenced by exercise, heat, illness, and stress. Normally they worsen in the evening and get better after resting.
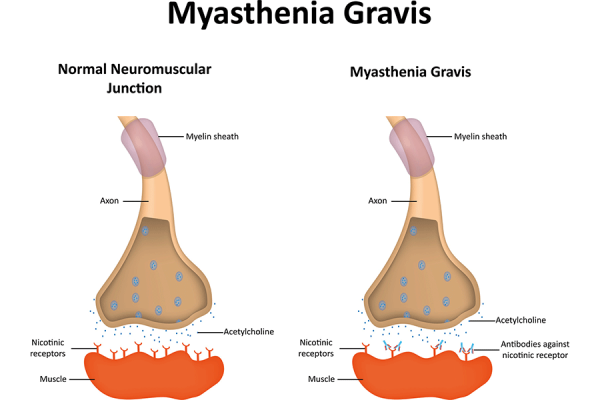
Causes
Often myasthenia gravis is associated with other disease like rheumatoid arthritis, scleroderma and systemic lupus erythematosus. 65% of patients with myasthenia gravis have a hyperplasia of the thymus. 15% of patients with myasthenia gravis present a Thymoma.
Diagnostic procedures
Myasthenia gravis is a clinical diagnosis by specialized neurologist, supported by specific tests including Cholinesterase inhibitor tests, antibody detection test, EMG (Electromyography), Computed tomography (CT) and MRI of the chest, to detect thymoma or thymic hyperplasia.
Treatment
The treatment of Myasthenia gravis is effective and most patients are able to live normal lives. Based on the clinical findings it could include certain drugs (Cholinesterase inhibitors, Immunosuppressant agents, Intravenous immune globulin (IVIG)), Plasmapheresis, Thymectomy, Physical therapy and Lifestyle changes.
Our Team Of Experts
Since more than ten years GNC is the leading clinic for Neurology in the UAE. All our Myasthenia Gravis experts are German Board Certified and have minimum professional experience of 25 years. If you are searching for the most trusted Myasthenia Gravis experts, you came to the right place.
Testimonials
``The doctor is the best and everyone's very helpful``
``Excellent doctor``
``I am thankful for the service.``
``Being able to have blood tests and EEG done at the clinic itself was very helpful and convenient. This also allowed my doctor to have fast access to the test results.``
``I'm impressed by the Professor and team professionalism``
``God bless you guys wish you more of success``
``Great service``
``It was a great visit thanks! It really helped me.``
As Seen On


Nerve Pain & Damage
Squeezed Nerve, Pinched Nerve, Compressed Nerve, Trigeminal Neuralgia
In their anatomical course through the body and the limbs nerves might be damaged in various ways, the cause of damage most often being traumatic. Symptoms of nerve damage may be prickling, numbness and pain but also palsy or disorders of the bladder or the rectum. Lower back pain is one of the most common complaints today. Up to 80% of the US-Population will suffer from back pain at least ones in their lives. Back pain or lumbar pain is the largest cause of work-related absence in the United Kingdom.
Trigeminal neuralgia
Trigeminal neuralgia is a special case of nerve pain. It is often described as the “the world’s worst pain.” Typically, patients suffer from attacks of intense, electric shock-like facial pain along the trigeminal nerve. More information here: Trigeminal neuralgia
Causes & Risk factors
Very often nerves are trapped at the spinal cord, the backbone or in their course to the limbs. The reason for this may be some injury, a slipped disk or the trapping of a nerve in a bony or connective tissue canal. A typical example is the carpal tunnel syndrome.
Symptoms
The symptoms are depending on the location of the injured or damaged nerve. Often nerves in the cervical or lumbar back are squeezed by a slipped disk causing neck or back and leg pain. Another common location is the wrist. If a nerve is squeezed here it results in pain in the hand called Carpal Tunnel Syndrome. But many other conditions can cause nerve damages in different locations such as sports related injuries of the shoulder and others.
Diagnosis
Most important is a consultation with an experienced Neurologist. The clinical impression and physical examination are guiding the way. If the location is identified, certain nerve tests like Nerve Conducting Velocity or Electromyography may be used to verify the diagnosis or to determine the location precisely.

Treatment
All conservative treatment options should be tried before a surgical intervention is considered. These treatment options also depend on the location of the damaged or squeezed nerve. Often specialized physiotherapy, certain braces and life style adjustments are successful. Moreover, an adequate pain management and other medications are essential to optimize a fast recovery. Most nerve damages are successfully treatable without surgery.
Our Team Of Experts
Since more than ten years GNC is the leading clinic for Neurology in the UAE. All our Nerve Damage experts are German Board Certified and have minimum professional experience of 25 years. If you are searching for the most trusted Nerve Damage experts, you came to the right place.
We can also help you with the best psychologist, psychiatrist and psychotherapist available in Dubai, UAE.Testimonials
``The doctor is the best and everyone's very helpful``
``Excellent doctor``
``I am thankful for the service.``
``Being able to have blood tests and EEG done at the clinic itself was very helpful and convenient. This also allowed my doctor to have fast access to the test results.``
``I'm impressed by the Professor and team professionalism``
``God bless you guys wish you more of success``
``Great service``
``It was a great visit thanks! It really helped me.``
As Seen On


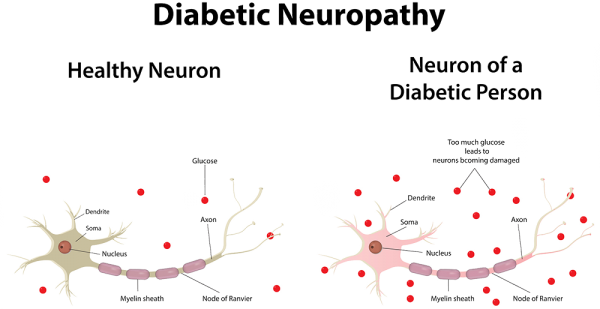
Neuropathy – Diabetic Polyneuropathy
Neuropathy - Polyneuropathy
Neuropathy is term that describes a damage of the nerves. Most common symptoms include: pain (often worse at night), numbness, tingling, ‘pins and needles’, burning sensation, muscle weakness and others. The damage can be caused by different conditions such as disease, infection, injury, medications, toxins or another reason.
Types of neuropathy
• Peripheral neuropathy affects nerves in outer (peripheral) parts of the body such as the feet, legs, hands and arms.
• Proximal neuropathy affects the muscles of the hips and the shoulders.
• Focal or mononeuropathy affects only one nerve. An example is carpal tunnelsyndrome.
• Polyneuropathy affects several nerves. Most people with neuropathy have polyneuropathy.
• Autonomic neuropathy: Nerves of the autonomic nervous system are damaged leading to symptoms such as problems with digestion, blood pressure and bladder function.
• Diabetic neuropathy is caused by diabetes most commonly affects the nerves of of the hands and the feet. It can also affect nerves controlling automatic functions of the body, such as digestion, or nerves in the hips and thighs.
In the UAE Diabetic Polyneuropathy is the most common type. Therefore, we will describe this type below more extensively.
Diabetic Neuropathy
60-70% of people with diabetes are suffering from Diabetic Neuropathies. Neuropathy may be present even before diagnosing diabetes. Diabetes is the most common cause of peripheral neuropathy in the world. However, the symptoms of neuropathy are mostly unknown to the patients and difficult to diagnose. Early diagnosis is important as diabeticneuropathy can damage any nerve in the human body. Be it the nerves controlling the heart beat or the nerves of the skin. Diabetic skin lesions are the major cause of foot amputation.
Causes
Similar to the variety of symptoms there is also a large variety of causes for this disease. The most frequent reason is a metabolic disorder such as diabetes mellitus. But also hereditary disposition, toxic inhibition or paraneoplastic development can cause polyneuropathy.
Signs & Symptoms
Diabetic Neuropathy means the affection of many nerves due to very different reasons and it can therefore develop many different symptoms. Most frequent are paraesthesia such as prickling, numbness, burning of the feet, but also palsies, disorders of speech and failure of cerebral nerves.
Types of Diabetic Neuropathy
There are different types of neuropathy with different typical patterns of pain distribution. For instance there is the:
Read MoreSymmetric type of diabetic neuropathy
Characterized typically by sensory loss, weakness and painful burning of toes and feet. First symptoms of the symmetric polyneuropathy may appear in the sole of one foot or even involving half a toe, then gradually spreading circumferentially up both legs to the knees, then into thighs and finally the hands. The latter pattern is also termed as “stocking-glove” distribution. Neuropathy always is length-dependent, because the longest axons are the most vulnerable. Patients describe tingling, prickling, burning, numbness and a band like pressure.
Due to sensory deficits, small cuts and wounds will not be noticed by the patients at first thus causing seemingly inexplicable infections. Later, weakness of the muscles will develop, particularly expressed by the fact that patients cannot stand on their heels. With progressing sensory disturbances spreading up also into the tips of the fingers, patients will have difficulties holding objects. Most common is a painful burning in the feet which gets worse with high temperatures. Light stimuli applied to the numb areas may be experienced as extremely painful. Also an imbalance of the gait, getting worse in the dark, is a common symptom of patients with Diabetes.
When the onset of diabetes occurs at a juvenile age of the patients, neuropathies may be first noticed as late as in their thirties to fifties but when the onset takes place at an age over 50, they tend to occur readily with adult-onset. There is a known correlation between the occurrence of neuropathy, the duration and the severity of diabetes, body weight, body size and long-standing hyperglycaemia which must be investigated individually with each patient.
Apart from the above described symmetric form of neuropathy there are other diabetes related neuropathies in different classifications:
Asymmetric diabetic neuropathy
showing focal weakness or sensory loss of single nerves, mainly in one upper arm, one thigh or the cranial nerves.
Asymmetric focal and multifocal types of diabetic neuropathy
of neuropathy are less common, but quite dramatic. They are usually acute in the onset with strong muscle weakness and pain in a thigh or upper arm, but this form rarely occurs before the age of 45. The affection of the cranial nerves causes weakness of the eye muscles accompanied by double images or facial numbness and nerve paralysis.
Autonomic dysfunctions in diabetic neuropathy
Many patients with Diabetes also develop dysfunctions of the autonomic nervous system: constipation, diarrhoea (particularly during the night,), abnormal sweating, hypertension, Tachy- and Bradycardia, dysfunction of the bladder and sexual impotence in males. Symptoms are also uncertain gait, imbalance, maybe syncope’s and blurred vision from lack of papillary regulation.
The distinction between the different kinds of diabetic neuropathy is crucial as far as the different approaches to diagnosis and management are concerned, but also regarding the prognosis.
Treatment
Accordingly, diagnostics and therapy of polyneuropathies are manifold and difficult. The therapeutic aim must be to prevent the deterioration of the nerves itself on the one hand and to treat the illnesses causing polyneuropathy on the other hand. The most essential parts of the evaluation of diagnosis and therapy are...
Read MoreThe most essential part of the evaluation of diagnosis and therapy are – apart from an intensive neurological examination – the electro diagnostic studies of the nerves. The examination comprises Electromyography (EMG) and nerve conduction velocity (NCV). The EMG involves recording electrical potentials by an electrode placed into the muscle, both at rest and during voluntary contractions. The NCV is carried out by stimulating the motor and/or sensory nerves electrically. From the data recorded, informative characteristics of the recorded forms of waves can be determined, thus leading to a clear picture and appropriate treatment.
In the long-term, by way of Diabetes and Complications Control, trial patients who controlled their diabetes meticulously showed significantly less neuropathy. When symptoms of neuropathy occur in patients suffering from diabetes or early signs of polyneuropathic painpatterns as described above, occur, an early neurological examination is of the essence.
Moreover, specialized neuropathic pain treatment can easy the symptoms. Common pain killers are usually not effective enough and anticonvulsants, antidepressants and other drugs need to be used.
Our Team Of Experts
Since more than ten years GNC is the leading clinic for Neurology in the UAE. All our Neuropathy experts are German Board Certified and have minimum professional experience of 25 years. If you are searching for the most trusted Neuropathy experts, you came to the right place.
Testimonials
``The doctor is the best and everyone's very helpful``
``Excellent doctor``
``I am thankful for the service.``
``Being able to have blood tests and EEG done at the clinic itself was very helpful and convenient. This also allowed my doctor to have fast access to the test results.``
``I'm impressed by the Professor and team professionalism``
``God bless you guys wish you more of success``
``Great service``
``It was a great visit thanks! It really helped me.``
As Seen On


Book Appointment
Parkinson’s Disease
Disease
What is Parkinson’s Disease?
Parkinson’s disease is a progressive neurodegenerative disorder characterized by rigidity, tremor, postural instability, and slowness of movement. It develops gradually, sometimes starting with a barely noticeable tremor in just one hand. Very often the changes in movement are very discreet and therefore an early diagnosis is often difficult. The disease commonly causes stiffness or slowing of movement. Although Parkinson's disease can't be cured, medications may markedly improve the symptoms.
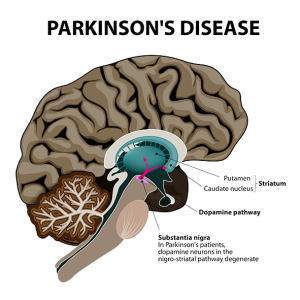
Disease
Symptoms
Parkinson’s disease symptoms may be mild at the beginning and often start on one side of the body. The signs and symptoms may include:
- Tremor (Shaking of the hands)
- Slowed movement
- Muscle stiffness
- Impaired posture and balance
- Loss of automatic movements
- Speech and writing problems
There may be other symptoms such as a reduction of superior intellectual brain functions, psychic symptoms such as Depression but also disorders of vegetative bodily functions.
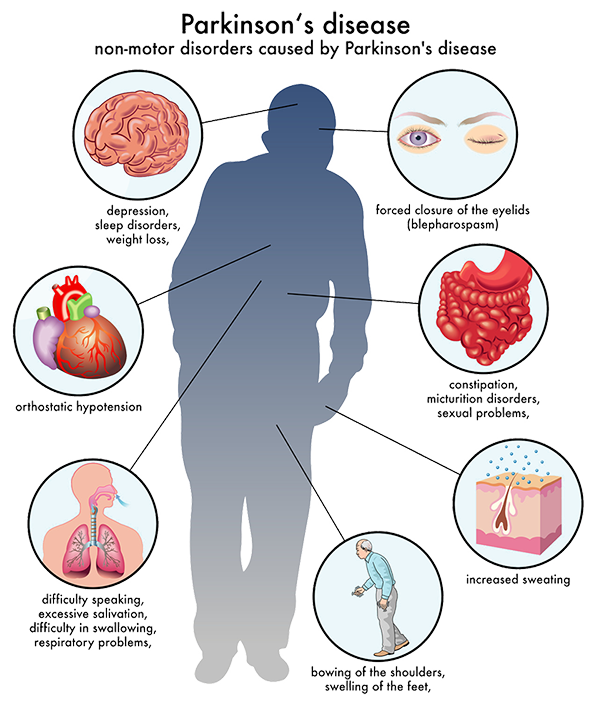
Disease
Causes
In Parkinson's disease, certain nerve cells (neurons) in the brain gradually break down or die. These certain nerve cells are responsible for the design, the development and the realization of movements. The loss of neurons results in a decreased dopa level in the brain. Dopa is a chemical messenger between nerve cells. The causes of Parkinson’s disease are not known but factors such as genes and environmental triggers may play a role. However, men are more likely to develop the disease than women are and it usually starts around age 60 or older.
Diagnosis
Early diagnosis of Parkinson’s Disease may be difficult as the symptoms are often subtle. The Neurologist will do a comprehensive history and physically examination and order tests to rule out other conditions that may be causing the symptoms. In addition he may give a certain Parkinson's disease medication. Significant improvement with this medication will often confirm the diagnosis of Parkinson's disease.
Treatment
So far, there is no cure for Parkinson’s disease but certain medications can help control the symptoms. They can help manage problems with walking, movement and tremor by increasing the brain's supply of dopa. Depending on the stage of Parkinson’s Disease and the age of the patient different medications are indicated. Certain medications have only a limited effect for a few years. If the effect is not sufficient anymore the medication needs to be augmented or changed.
The main focus of the treatment will be on adequate medication and physiotherapy. Physical exercises are useful therapeutic means. In severe cases neurosurgical intervention might be necessary which is known as deep-brain-stimulation. The surgeons implant electrodes into a specific part of the brain and connect them to a generator implanted in the chest near the collarbone that sends electrical pulses to the brain. Deep-brain-stimulation may reduce Parkinson's disease symptoms.
Living with Parkinson’s disease
It is necessary that the patient works closely with the Neurologist to find the right treatment. Certain lifestyle changes such as a healthy diet and physical exercises may help make living with Parkinson's disease easier. Walking, swimming, dancing, water aerobics or stretching is recommended in order to improve the balance which could be disturbed by the disease. Moreover, some types of alternative medicine such as meditation, yoga, massage, tai chi and acupuncture could be useful tools.
We can also help you with the best psychologist, psychiatrist and psychotherapist available in Dubai, UAE.
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
Restless Legs Syndrome
Disease
What is Restless Legs Syndrome?
Restless Legs Syndrome (RLS) is a neurological disorder characterized by an extremely uncomfortable feeling such as creeping, throbbing, pulling, itching or needles and pins in the legs, typically in the evenings while sitting or lying down. It makes the patient feel like getting up and moving around which reliefs the unpleasant feeling temporarily. Restless Legs Syndrome mostly affects the legs, but can also affect the arms, torso, head, and even phantom limbs. It can disrupt sleep and thus leading to daytime drowsiness.
RLS symptoms often begin at the age of 40 years but up to one-third of patients develop symptoms before the age of 20 years. RLS affects estimated 7 to 10 % of the young to middle aged people and 10 to 20 % in those older than 60 years. In the Middle East region approximately 3% of the general population is affected. It is twice as often in women as in men. Especially pregnant women suffer from RLS. 25% of pregnant women develop the disorder in the last three month of pregnancy.
Symptoms
Restless Legs Syndrome symptoms are most commonly located in the deep of the calves, in the feet and thighs. Initially the patient often get an exaggerated sense of positional awareness of the affected leg, later the sensations appear or intensify even while sitting. Movement of the affected part of the body, for instance walking around brings an immediate relief, although temporary and partial and the sensations immediately return after the movement stops. These symptoms often lead to a severe sleep deficiency with secondary tiredness and loss of concentration in job or while driving a car. Some people with severe RLS are not even able to go to work.
Causes
One distinguishes between two kinds of Restless legs Syndrome: the primary and the secondary RLS.
The primary (idiopathic) RLS is a neurological disease with unknown causes. A disturbance of a neurotransmitter system in the brain is suspected. Medication which interferes with the neurotransmitter system helps reliably.
The secondary (symptomatic) RLS is most commonly associated with iron deficiency, venous disorders, polyneuropathy, folacit deficit, Diabetes, renal diseases or pregnancy.
Restless Legs Syndrome can also be induced by antiemetic, anti-depressive and anti-psychotic drugs. A primary RLS should not be considered until possible medical conditions are ruled out, especially venous disorders and polyneuropathy.
Risk Factors
1. AGE. The syndrome affects 10 percent of people 65 and older, compared with only 5 percent of the general population.
2. SEX. Women are more likely to experience the condition than men, but the sex connection seems to be tied to pregnancy. If a woman has never been pregnant, her risk is the same as a man's.
3. LOW IRON. Diminished iron in the brain is implicated in the syndrome.
4. FAMILY HISTORY. People with a family history of the disease are at greater risk.
More than just a discomfort
Harvard researchers found out that sleep deprivation – caused by Restless Legs Syndrome (RLS) – leads to higher risk of early death. Former studies linked RLS with many other conditions, including depression, high blood pressure, and heart disease. This shows that RLS is not just a discomfort or a condition causing sleep problems. It has severe effects on overall health and longevity.
Treatment
The goal of a treatment of Restless Legs Syndrome is to reduce the uncomfortable sensations. Sometimes it is necessary to treat underlying conditions such as iron deficiency or peripheral neuropathy.
With Medication
To reduce the restlessness in the legs there are several medications available such as medications for Parkinson’s disease which reduce the amount of motion in the legs by affecting the level of the neurotransmitter in the brain. Moreover, medications for Epilepsy may help reduce the uncomfortable feeling, as well as muscle relaxants and sleep medications. But these medications don't eliminate the leg sensations, and they may cause daytime drowsiness.
Without Medication
Iron place a big role in Restless Legs Syndrome. Iron levels should be measured and a deficiency should be balanced. Furthermore, a non-medical therapy includes the avoidance of caffeine, alcohol, nicotine, and medications that exacerbate Restless Legs Syndrome, physical activity and good sleep hygiene. Simple lifestyle changes often play an important role in alleviating symptoms of RLS and to learn some relaxation techniques such as yoga and meditation can lead to a significant improvement.
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
Sciatica
Sciatica
Sciatica is a common neurological condition described as pain, numbness, weakness, or tingling radiating from the lower back to the leg. The symptoms usually occur on one side and vary from mild to unbearable.
It is important to understand that sciatica is not a disease itself. It is rather a symptom caused by an underlying condition. In most cases the underlying condition is a herniated disc, other degenerative disc diseases or spinal stenosis.
The treatment depends on the underlying conditions. Usually Sciatica has a very good prognosis if the treatment is started early enough.
Causes
Sciatica can be caused by any underlying condition that squeezed the sciatic nerve. The sciatic nerve is a large nerve that starts in the lower back and runs down the back of each leg. It controls the muscles and the sensation of the leg and foot.
Read MoreConditions that may cause sciatica
• Bulging or herniated disk in the back (most common)
• Other degenerative disk disorders
• Lumbar spinal stenosis
• Piriformis syndrome
• Tumor and others
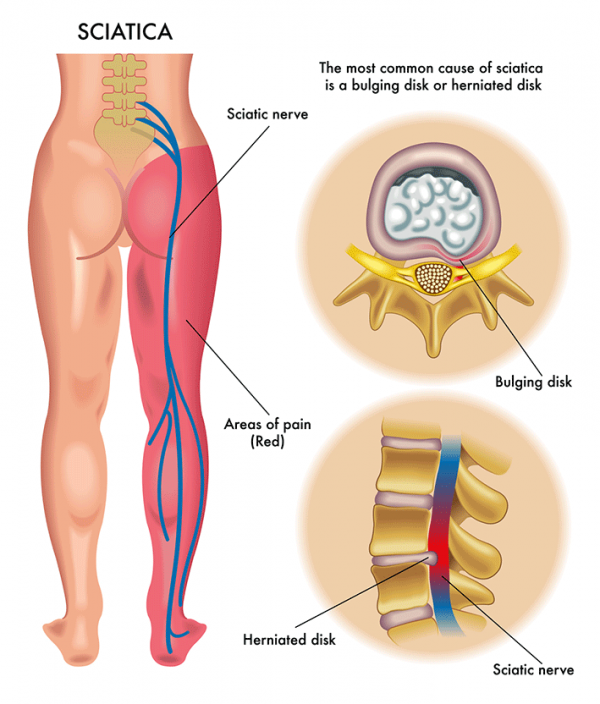
Signs & Symptoms
The symptoms are depending on anatomical structure and the function of the sciatic nerve (see above). The following symptoms may occur in the lower back, the buttock, the hip and the leg:
Read More• Pain: Often the pain is described as a sharp pain. The pain can be so severe that movements may be difficult.
• Tingling, burning, numbness or other sensory symptoms
• Weakness of the muscles and problems to move the leg
Symptoms may worsen when you cough, sneeze, or laugh, or when you sit or stand for long periods of time. Being overweight is a risk factor.
Treatment
As a first step, it is important to find the underlying condition causing the sciatica. A neurologist can find the location of the lesion by the symptoms presented. Depending on the location (L4, L5, S1) symptoms in the leg may vary. The treatment depends on the underlying condition and the severity of symptoms. If the symptoms are very mild and there is no danger of worsening, the symptoms may improve on its own.
Depending on the underlying condition the treatment may include:
Read More• Medication: Most patients need pain relieving medication. Moreover, medication that relaxes the muscles and thus reduces the pressure on the nerve may help as well.
• Physiotherapy: Initially it is important to reduce any movement that puts pressure on the sciatic nerve. Moreover, strengthening and stretching exercises may applicable. Applying heat or icing brings relief in some patients.
• CBT: Large studies could show that Cognitive behavioral therapy is effective in reducing the pain and coping with the symptoms.
• Injections: In severe cases injections that reduce the pain and inflammation may help.
• Surgery: Surgery should always be the last option and is not required in the vast majority of cases.
Read more about specific treatment of slipped or bulging disk here.
Prognosis
Usually sciatica has a very good prognosis. The sooner the underlying condition is diagnosed and the sooner the correct treatment starts, the better the outcome.
Our Team Of Experts
Since more than ten years GNC is the leading clinic for Neurology in the UAE. All our Sciatica experts are German Board Certified and have minimum professional experience of 25 years. If you are searching for the most trusted Sciatica experts, you came to the right place.
Testimonials
``The doctor is the best and everyone's very helpful``
``Excellent doctor``
``I am thankful for the service.``
``Being able to have blood tests and EEG done at the clinic itself was very helpful and convenient. This also allowed my doctor to have fast access to the test results.``
``I'm impressed by the Professor and team professionalism``
``God bless you guys wish you more of success``
``Great service``
``It was a great visit thanks! It really helped me.``
As Seen On


Stroke
Disease
Stroke, CVA (cerebrovascular accident), CVI (cerebrovascular insult), Brain Attack
Definition
Ischemic stroke, also known as CVA (cerebrovascular accident) or CVI (cerebrovascular insult) or Brain Attack is defined as an interruption of blood flow within one of the brain feeding arteries. Thus the effected brain areas are losing their function and if not treated in time, the nerve cells are dying. Depending on the affected area a stroke can have various clinical signs.
Causes & Risk factors
Most common causes of an ischemic stroke or CVA (cerebrovascular accident) are arteriosclerosis and cardiac embolism following atrial fibrillation. Other causes are vasculitis, arterial dissection or diseases causing hyper-coagulation (blot clotting). There are certain risk factors associated with ischemic stroke or CVA (cerebrovascular accident): age over 60, male gender, Hypertension, Atrial fibrillation, Diabetes mellitus, Dyslipidemia, Cigarette smoking, Migraines.
Symptoms
Symptoms of an ischemic stroke or CVA (cerebrovascular accident) are depending on the affected area of the brain. Often symptoms occur suddenly and are affecting one side. It could be sudden loss of vision, weakness of a limb (paresis), numbness or loss of sensory, problems speaking or swallowing, loss of consciousness, headache, nausea and others. If the symptoms fully recover, the neurologist speaks about an TIA, transient ischemic attack.
Diagnosis
Ischemic stroke or CVA (cerebrovascular accident) is a clinical diagnosis. However, the following tests need to be performed. CT scan or CT angiography, MRI, ECG (Electrocardiography), ECD (Extracranial Duplex Sonography), TCD (Transcranial Duplex Sonography), Echocardiography, blood examinations.
Treatment
The most effective treatment is the prevention of an Ischemic stroke or CVA (cerebrovascular accident). This means reducing the risk factors. To evaluate the risk of Carotid artery stenosis a neurologist can perform a ECD (Extracranial Duplex Sonography), TCD (Transcranial Duplex Sonography). Depending on the findings patients can benefit from interventional therapy, such as carotid endarterectomy. Hypertension, Atrial fibrillation, Diabetes mellitus, Dyslipidemia must be monitored closely and treated correctly. Moreover life stile changes should include: Diet, sports, reducing smoking.
In case a stroke or CVA (cerebrovascular accident) happened, time is the most important factor. Patients must be admitted and treated in a hospital within 3h. First line therapy is i.v. thrombolysis in combination with other medication.
After a stroke or CVA (cerebrovascular accident) happened, patients must take medicine to prevent a second event. This medicine keeps the blood from clotting. Moreover early rehabilitation is determining the recovery. The rehabilitation must be comprehensive and include physiotherapy, speech therapy, occupational therapy and psychology.
Other than that if you think your problem can be solved by a psychiatrist or a psychologist, you can book an appointment with them as well.
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
Tingling, Numbness, Weakness, Pain
You are experience tingling, numbness, weakness or pain and you want to know what’s causing it? This quick guide will explain you how.
Tingling & Weakness in Hands, Feet, Legs Treatment: Symptoms & More
A disease is the underlying cause (i.e. multiple sclerosis), a symptom is how the disease presents itself (i.e. numbness in the limbs)
Tingling, numbness, weakness and pain are the most common symptoms in neurology. Why? Neurology is the science of the nerves (neurons). There are different types of Nerves in the human body:
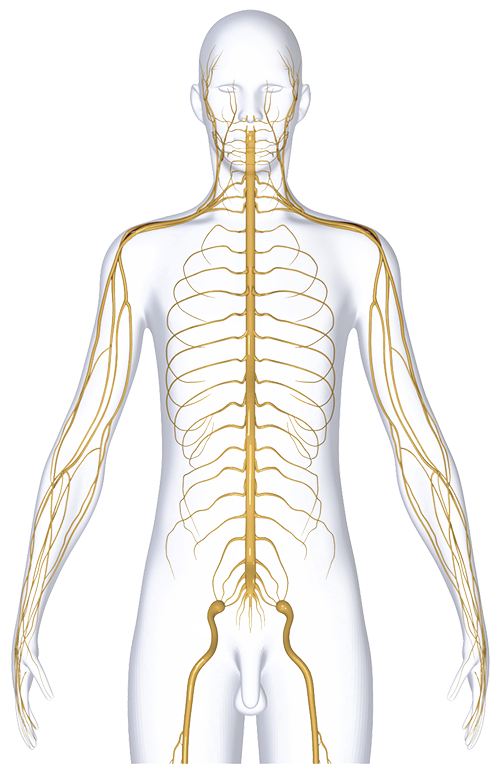 Sensory (or afferent) neurons: send information from sensory receptors to the brain. The receptors have different locations and functions:
Sensory (or afferent) neurons: send information from sensory receptors to the brain. The receptors have different locations and functions:1. Eye - Vision
2. Nose – Smell
3. Tongue – Taste
4. Skin, inner organs – Feel, Vibration, Pressure, Pain
Motor (or efferent) neurons: send information from the brain to muscles or glands.
1. Muscles (limbs, heart, blood vessels etc..)
2. Glans (saliva etc..)
The nervous system is controlling all functions of the human body. A nerve damage is resulting in a specific function loss
1. Numbness: damage of a sensory nerve sending sensory information from the skin to the brain
2. Tingling: damage of a sensory nerve sending sensory information from the skin to the brain
3. Pain: damage of a sensory nerve sending sensory information from the skin to the brain
4. Muscle weakness: damage of a motor nerve sending a movement impulse from the brain to the muscles
Ok, tingling, numbness, weakness and pain are the most common symptoms in neurology and they are caused by nerve damages. So far so good. Now it gets a bit more complicated because we want to know where and which exact nerve is damaged. Basically there are 2 different locations possible. The CNS (Central Nervous System – Brain & Spine) and the PNS (Peripheral Nervous System – Nerves of the limbs and inner organs). It’s a bit confusing because:
Both locations can lead to the same symptoms you may experience.
For example blindness. The patient is suffering from vision loss. This can be caused by a damage of the nerve receptors in the eye, the nerve cells leading from the eye to the brain or the nerve cells in the brain itself. Tingling, numbness or pain can be caused by a damage of the nerve receptors in the skin, the nerve cells leading from the skin to the brain or the nerve cells in the brain itself.
Now it gets even more complicated because we want to know the cause of the nerve damage.
The same symptom can be caused by many different diseases.
Numbness can be caused by a squeezed nerve, by neuropathy, by multiple sclerosis or by a brain tumor etc. This shows why it is important to find the exact cause of the nerve damage.
Causes
• Multiple sclerosis
• Stroke, Transient ischemic attack (TIA)
• Migraines
• Seizures
• Nerve Damage (Neuropathy) due to Diabetes
• Nerve injury (i.e. neck injury, back injury)
• Herniated disk in your spine
• Pressure on your nerves (could be due to scar tissue, enlarged blood vessels, infection, tumors or Carpal tunnel syndrome (pressure on a • nerve at the wrist)
• Sitting or standing in the same position for a long time
• Transverse myelitis (inflammation of the spinal cord)
• Encephalitis (inflammation of the brain)
• Abnormal electrolyte levels
• A lack of vitamin B12 or other vitamin
• others
The treatment will be completely different depending on the cause.
Summarizing, we know that tingling, numbness, weakness and pain are the most common symptoms in neurology and they are caused by nerve damages. The damages can be in different locations and they may be caused by different underlying diseases.
How does a neurologist find out what is causing my tingling, numbness, weakness and pain?
In the consultation he will ask you about the symptoms you are experiencing. Onset, pain level, changes during the day or night time, development, location etc… In the neurological examination he will investigate the symptoms and check if they are on both sides, limited to a dermatome, reflexes etc. Moreover for specific damages there are specific neurological examinations like NCV (nerve conducting velocity), Evoked Potentials, MRI etc. Certain diseases like multiple sclerosis require more extensive investigations.
We hope this article could give you a short and not too medical overview of the diagnostic process in case you are experiencing the most common neurological symptoms of tingling, numbness, weakness or pain. In case you have further questions, our team also consists of experienced doctors in psychology, psychiatry and psychotherapy. Please don’t hesitate to contact us.
Traumatic Brain Injury (TBI)
Traumatic brain injury (TBI) is a consequence of head injury in which a blow to the head results in damage to the brain due to stretch forces. TBI is the leading cause of death in North America for people below 45 years. The UAE has a comparably young population which makes TBI a very common and serious disease.
Many survivors live with significant disabilities, resulting in major socioeconomic burden as well. In 2000, the economic impact of TBI in the US was estimated to be $9.2 billion in lifetime medical costs and $51.2 billion in productivity losses.
Symptoms are often mild and hard to detect. It needs a trained specialist to diagnose and most importantly treat the condition. If treated adequately TBI has very good prognosis.
Causes
• Motor vehicle accidents
• Sport Injuries
• Falls
• Violence
• Military combatSymptoms
Brain injury is a frequently misunderstood injury. Numerous invisible residual complaints are labelled as 'psychological' and are not well understood. A major complaint of brain injury is fatigue and overstimulation.
Overstimulation
We live in a society that is very fast, with lots of stimuli to be processed at a high speed. When someone experiences overstimulation it is harder for them to process stimuli, sounds are perceived as louder and light as brighter. Ambient noise is perceived as irritating, normal sunlight is harder to endure and one gets easily overwhelmed by crowds and lots of movements in their surrounding.
Fatigue
Due to the quick onset of fatigue it can be difficult to go to birthday parties, to go grocery shopping and to participate in social activities. The fatigue causes disturbances in thinking processes and limits the entire functioning. After reading a text, one can already be so tired that one must rest for a period to recover from the mental effort. In particular, the reading of displays (smartphone, computer, tablet) can be highly discomforting to patients who experience brain injury. In addition to the fatigue and overstimulation one notices to have more trouble remembering and concentrating. Memory and concentration becomes harder when fatigue increases.
Secondary Symptoms
When one experiences symptoms but keeps on functioning beyond their own capacity, people can develop secondary complaints. Overstimulation of the brain cannot be compared to overstimulation of the body. The body has, for example, pain signals as a warning signal. The brains gives totally different warning signals like overstimulation by light, noise or crowds, having difficulty processing stimuli, more problems with thinking (concentration and memory) and fatigue. Many people do not recognize these alarm signals, or are not adequately dealing with them and are likely to push through their complaints. The functioning outside their own capacity will further increase the complaints and ultimately exhaustion will occur. Not being able to function in the way as is desired by the patient, the patient can also develop emotional reactions which are often characterized by feelings of powerlessness and frustration. Misunderstood injury thus consists of fatigue, rapidly becoming overstimulated, experiencing a decline in performance and emotional responses.
Misdiagnosing Traumatic Brain Injuries
Brain injury patients are often misdiagnosed or not diagnosed at all. As most professionals are not specialized in diagnosing TBI, the patients hear often “there is nothing wrong”, even if they are suffering from symptoms. Or their symptoms are evaluated as “only psychological”. Not treating TBI adequately will worsen symptoms. This described process is resulting in a major socioeconomic burden (US: $9.2 billion in lifetime medical costs and $51.2 billion in productivity losses).
Diagnosis
Neuropsychological assessment is needed to get a good impression of the 'invisible' residual symptoms and how to cope with them. The neuropsychological examination is used to assess the extent of (mental) energy loss, fatigue, cognitive - / emotional changes and the impact of pain sensations.
At the start of the counseling / therapy an extended interview (anamnesis) with the patient is performed. A broad range of issues are discussed, such as what happened, what are the symptoms, has it been a breaking point in the health perception, which conditions worsen symptoms or affect it. Furthermore, we look at (medical) history, education, type of work, hobbies, social life and how complaints are limiting it. A neuropsychological examination is carried out and on the basis of the results an appropriate treatment plan is suggested. If there is not enough information available, the expertise of many other disciplines can be consulted (neurologists, internists, psychiatrists, etc.).
With this information and understanding, it is possible to establish an adequate treatment involving persons with brain injuries to understand the actual limitations and how to adapt to it.
Treatment
It is important to know that patients themselves often do not have a good understanding of the limitation of their symptoms and complaints, and the patient is driven to perform at pre-morbid level. Recovering from brain damage is a complex process that a patient has to go through with the help of a professional. It is necessary that one acquires knowledge in the presentation of symptoms and also get advice how to deal with it. A brain injury is essentially a neuropsychological phenomenon.
Neuropsychological Rehabilitation
In the next phase, the affected cognitive functions are reactivated and a medical fitness program is used to improve the energy level and reduce pain levels.
Often, the treatment consists of guidance of a clinical neuropsychologist which will provide insight into the complaints and why these occur. Adjustments are taught and exercise / rest schedules are discussed. During the same period, patients will follow medical fitness programs and a cognitrain program. This followed by rest periods. If pain symptoms stay apparent, a neurologist or pain doctor (anaesthesist) is considered. Often the pain sensations consist of pain in the neck and shoulders which also develops into headaches. The progress of each patient is discussed daily and programs are adapted to this feedback. The goal is to become a well- balanced individual again.
To achieve this, the main focus is on personal attention. Our view is that every person is like a fingerprint, completely unique. There is no standard protocol used to provide treatment, as each person has their own way of reacting to all aspects relating to brain injury.
The program usually has a duration of three months and the maximum group size is 12 people. The main goal of a small group is to build a personal relationship with each participant in the program.
If you think that you want to fix something else related to your mental health. GNC Dubai is providing one of the best psychiatrists in Dubai, psychologists in Dubai and psychotherapists in Dubai who can help you find the core reason and in fixing it.
Common Misconception
Often there is a misconception that the complaints of (mild) brain injury will resolve after some time. This natural recovery can only occur when conditions are optimal. One needs to perform the right activities during the recovery period in order to optimize the recovery. It should be noted that even with an optimal recovery period there may be residual complaints!
Vertigo
Disease
Vertigo, Dizziness, Giddiness, Lightheadedness
Approximately 15% of the population is suffering from dizziness, vertigo, imbalance, lightheadedness, giddiness or unsteadiness. Vertigo is the perception of movement without actual movement (illusion of motion). Most commonly it is the sensation of spinning (either the room spinning or the person spinning). But it can be the sensation lateral movement, swaying or tilting, too. Vertigo is a type of dizziness. However, dizziness could also include other symptoms which not necessarily come with the feeling of spinning, such as imbalance, lightheadedness, giddiness and unsteadiness. Vertigo is a symptom, not a diagnosis. Meaning that vertigo can be caused by a wide range of diseases; from harmless to life threatening. In this article we focus on the most common neurological diseases.
Symptoms & Signs
Most commonly patients will experience the feeling of dizziness, vertigo, imbalance, lightheadedness, giddiness or unsteadiness. Moreover postural instability and feeling of falling or actual falling. Patients often need to sit or lie down and are suffering from nausea or vomiting. Ataxia (walking difficulties) and nystagmus (eye movements) could be present. Depending on the underlying cause the following symptoms could be present: hearing loss, tinnitus, ear pressure, visual problems. Moreover numbness of the skin, muscular weakness, coordination problems, speech or language difficulties, difficulty swallowing.
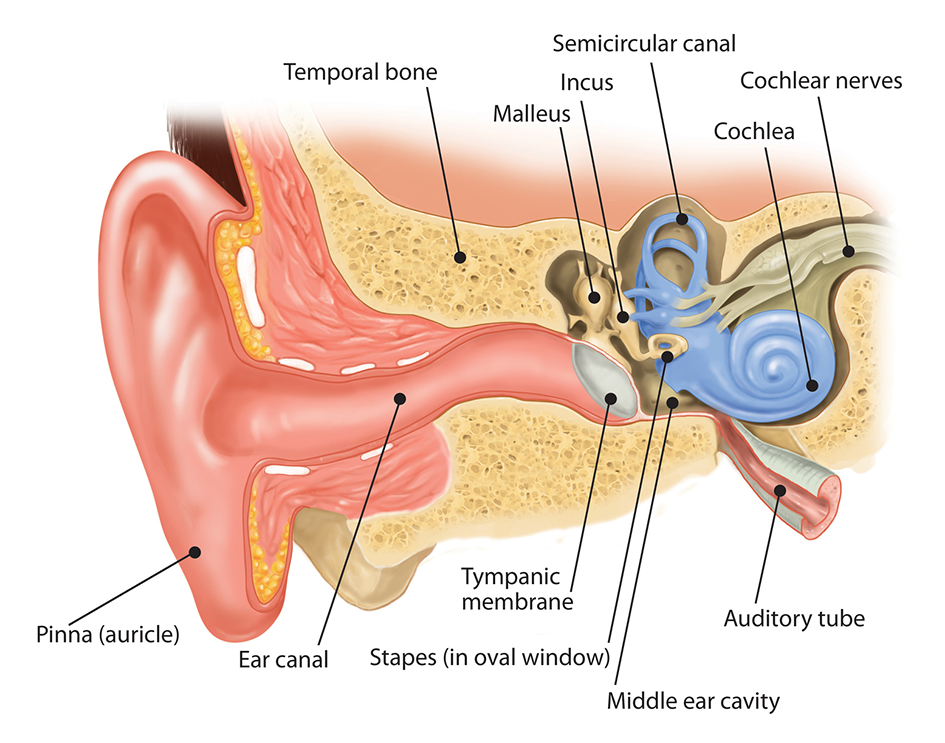
Causes
The causes of vertigo or dizziness can be manifold. There are various diseases that could cause the symptom of vertigo. It can be a disease of the ear or inner ear, the vestibular nerve or the brainstem. It could take comprehensive examinations to find out the real cause. Here we would like to highlight the most common causes.
1. Benign paroxysmal positional vertigo (BPPV): Benign paroxysmal positional vertigo is the most common cause of vertigo. Certain head movements can provoke a vertigo attack. The attacks are short (<30sec). Often the vertigo attack occurs in the night while rolling over in bed. This from of vertigo is caused by small crystals of calcium deposits in the ear canal that periodically become dislodged by specific head positions or movements. It is a very common form of vertigo.
2. Vestibular neuritis: Vestibular Neuritis is caused by an inflammation of the nerve to the semicircular canals, which helps control the balance. It is characterized by a sudden severe attack of vertigo, which lasts for seven to ten days.
3. Ménière disease: This disorder of the inner ear causes spontaneous episodes of vertigo along with fluctuating hearing loss. It is often attended by a Tinnitus (ringing in the ear) and a feeling of pressure or fullness in the ear.
5. Labyrinthitis: An inflammation of the inner ear structure called the labyrinth, caused by untreated bacterial infections of the middle ear. It can also cause loss of hearing.
6. Head trauma: A violent blow on the head can cause damage to the inner ear. This may lead to balance problems like Vertigo or Dizziness, temporary or permanent.
7. Others: Migraine, Superior canal dehiscence syndrome, Otitis media, Herpes zoster oticus, heart diseases and low blood pressure, Parkinson disease, Brain Stroke, Brain tumor, Acoustic neurome, Vestibular schwannoma, Epilepsy, Chiari malformation, Multiple sclerosis, Cholesteatom, Perilymphatic fistula, Superior semicircular canal dehiscence syndrome, Autoimmune disease, Psychological disorders like panic attacks or anxiety
Diagnostic procedures
First step should always be a consultation (important is the onset, triggers, duration, frequency, accompanying symptoms of the vertigo) and a comprehensive neurological examination (including coordination, nystagmus and gait testing). Only then a experienced neurologist can evaluate which further tests could be necessary. Such as Dix-Hallpike test, AEP, auditory evoked potentials, Vestibular evoked myogenic potentials, audiogram (hearing test), Tympanometry, Videonystagmography, Electrocochleography, Computed tomography (CT) or MRI
Treatment
The treatment of vertigo depends on the underlying cause. Only if the neurologist could find out the cause by the above mentioned procedures the treatment should start. If the cause is life threatening like an acute stroke immediate action has to be taken. Most commonly the treatment is not that urgent. In the following we give you a short overview of possible treatment options. However, which ones apply depends on the findings I the diagnostics.
1. Repositioning maneuvers for BPPV (eg Epley maneuver or Semont maneuver)
2. Pharmacotherapy: Vestibular suppressants (Meclizine, benzodiazepines), corticosteroids and diuretics, β-blockers, calcium-channel blockers, antidepressants, anticonvulsants.
3. Physical Exercise or physical therapy Generally speaking physical activity is positive because the inner ear gets trained by this. Dangerous situations or the risk of falling should be avoided of course.
4. Lifestyle: In case of migraine vertigo trigger situation should be avoided. Further migraine treatment cou can find here.
Professor Dr. med. Detlef Koempf – Neurologist & Expert for Vertigo & Visual Problems

Professor Koempf, Specialist for vertigo & visual Problems, is a genuine German University Professor born in Saeckingen, near Freiburg and studied medicine in Heidelberg.
After having spent one year of research in the USA, he continued his medical education at the University Hospitals Mannheim and Heidelberg and went on to work as Deputy Head at the Neurological Hospital in Erlangen.From 1987 until 2010, Professor Koempf held the position as Director of the Neurological University Hospital of Luebeck, Germany where he worked as a Senior Consultant for Neurology, held lectures and taught students. In 2010 he was elected as General Secretary to the EFNS (European Federation of Neurological Societies) where he organizes large neurological conventions and further education for neurologists in Eastern Countries such as Russia, Belarus, Ukraine, Moldavia and others.
Aim of these efforts is to standardize neurological diagnostics and treatment in Europe.In 1998, Professor Koempf wrote an important book on the topic of “Clinical Neuro-Ophthalmology”, vertigo and visual problems which was published by the renowned Thieme Publishers. He also deals with all “Diseases of the Cranial Nerves” on which he also published a book in 2006.Since finishing his Univerity career, Professor Koempf has been seeing patients in his private clinic in Luebeck and spends some months in Mallorca, Spain, in a Vertigo Center which he founded at Juaneda Hospital.
During his active time as Director of the Neurological Hospital at Luebeck University, Professor Koempf dealt with the whole range of neurological diseases including Parkinson’s disease, Epilepsy, Multiple Sclerosis, Cerebral circulatory disorders, stroke prophylaxis, disturbances of the memory, dementia, headaches, migraine, polyneuropathies, restles legs syndrome, back pain and diseases if the discs.But above all, he concentrated on the numerous kinds of vertigo (of which there are about 50) as well as vision disorders or disturbances of the equilibrium. Vertigo itself is just a very general term which does not mean anything specific. One must differentiate between specific vertigo meaning everything is spinning and unspecific vertigo which may mean short loss of vision, dizziness or disturbed equilibrium.The problem always is to find the underlying cause because very often the cause of very strong symptoms may be quite harmless whereas a slight symptomatology may indeed have a dangerous cause. In the latter case, a fast course of diagnostics is of the utmost importance in order to prevent for instance a stroke. The whole range vertigo lies between these two poles.The most important issue when dealing with vertigo symptoms is the medical history and the correct analysis of the symptoms. At the beginning of this procedure there will be a thorough neurological examination with a focus on the eye movements.
From time to time it will be necessary to carry out a psychiatric exploration as well because vertigo can be due to psychic problems. Following this will be neurophysiological investigations such as EEG, VEP, AEP or others and the DUPLEX ultrasound examination of the cranial arteries and a combined cooperation with an ENT doctor, an ophthalmologist, maybe an orthopedist and a qualified laboratory. Despite his being in Dubai only recently, Professor Koempf realized that all services he needs for his highly specialized work are available in Dubai, predominantly offered by German colleagues such as ophthalmology, ENT, orthopedics, cardiology and laboratory. This makes diagnostics and treatment easier since they all follow the same high German standards and uncomplicated communication between them allows secured results. Professor Koempf is devoting some of his time at the moment to meeting and getting to know these colleagues in order to guarantee best results for his patients. As main problems in this region, Professor Koempf notices so far the often faulty medicinal treatment of patients suffering from Parkinson’s disease or epilepsy, missing preventative measures for stroke and other diseases of the vessels as well as pain therapy regarding the numerous kinds of headaches or polyneuropathy caused by diabetes. Above all he is concerned about people suffering from dizziness and vertigo which is one of the most prevalent complaints presented in a neurological clinic and not to be underestimated regarding the possibly underlying serious causes.Professor Koempf will continue to inform us about the topic of vertigo on this site.
We can also help you with the best psychologist, psychiatrist and psychotherapist available in Dubai, UAE.
Book Your Appointment with Prof Koempf - Vertigo Expert
Saturday - Wednesday: 9am to 8pm Thursday: 9am - 7pm JLT Jumeirah Lake Towers, Cluster I, Platinum Tower 2806 Right side: 3hrs free parking Left side: all day free parking DHCC Dubai Healthcare City, Bld.
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)
© GNC, German Neuroscience Center Dubai (Neurology, Psychiatry, Psychology, Counseling, Dubai, UAE)